Baby stool with blood and mucus: Bloody Stools in Children
Posted onCopious amount of bloody stool in a newborn shortly after birth
- Journal List
- SAGE Open Med Case Rep
- v.9; 2021
- PMC8543549
As a library, NLM provides access to scientific literature. Inclusion in an NLM database does not imply endorsement of, or agreement with,
the contents by NLM or the National Institutes of Health.
Learn more about our disclaimer.
SAGE Open Med Case Rep. 2021; 9: 2050313X211054260.
Published online 2021 Oct 21. doi: 10.1177/2050313X211054260
,1,1,1,2 and 1
Author information Article notes Copyright and License information Disclaimer
Melena neonatorum is not uncommon; it presents as bloody stool in newborns and is caused by ingestion of maternal blood. This case presents an infant who had multiple episodes of copious amount of blood in his stool starting at 10 min of life, which raised multiple concerns requiring further investigation. The alkali denaturation test confirmed that the blood was maternal; however, due to the amount of bloody stool and the time required for the alkali denaturation test to result, further workups such as abdominal radiograph and hemoglobin/hematocrit were completed to ensure nothing was overlooked. Our infant remained clinically stable under the newborn nursery care, and did not require a higher level of care. He was discharged with his mother at 52 Hours of Life with a follow-up appointment the next day with the Primary Care Physician.
Keywords: Melena neonatorum, hematochezia, alkali denaturation test, bloody stool, swallowed maternal blood
Causes of bloody stool in neonates can range from benign, such as swallowed maternal blood, milk protein allergies, or anal fissures,1–3 to life-threatening, such as sepsis, gastrointestinal malformations, infectious colitis, necrotizing enterocolitis (NEC), arteriovenous malformations, and thrombocytopenia.
Maternal blood ingestion usually occurs perinatally, and it typically presents as maroon/coffee-ground emesis, maroon-colored blood in meconium, blood-streaked stools or melena.1–4 The alkali denaturation (Apt) test5
is the most appropriate test to determine if blood in stool is a swallowed maternal blood; however, this test is time-consuming and some hospitals do not even offer it in their labs. In these cases, the test must be sent out to another lab to perform it.
We present the case of a large amount of bloody meconium in a newborn as presentation of swallowed maternal blood, which is not well-described in the literature.
This case involves a 37 weeks gestational age (GA) male newborn delivered via spontaneous vaginal delivery to a 23-year-old mother gravida 1 para 1 whose blood type is O positive, Rh positive.
Pregnancy was also complicated by adequately treated syphilis diagnosed at 21 weeks GA with an appropriate response of fourfold drop in rapid plasma reagin (RPR) titers. Antenatally, labor was complicated by adequately treated Group B streptococcus agalactiae (GBS) colonization.
The placenta had a 3-centimeter sac-like structure attached to the lateral aspect of the placenta near cord insertion, which was described as a membranous sac with viable fetal organs (pancreas, bowel, and lymphoid tissue). Considering the patient’s history, imaging studies, and histomorphology, the findings are consistent with twin reversed arterial perfusion (TRAP sequence). There were no signs of placental abruption.
Infant’s APGAR scores were 8 and 9 at minutes 1 and 5, respectively,6
but at 10 min of life, the infant had a significant amount of grossly bloody meconium, which covered large parts of three baby-blankets.
Clinically, infant was well appearing and hemodynamically stable. Vital signs were reassuring: temperature 98.6°F, heart rate 130 per minute, blood pressure 55/30 mm Hg, oxygen saturation 99%, and weight 2890 grams. PE was normal.
Arterial cord gas: pH 7.04 and base excess −15.9 mmol/L which were consistent of in-utero acidosis. Capillary blood gas collected from the infant at 1 Hour of Life (HOL) resulted in spontaneous improvement in the acidosis: pH 7.31 and base excess −5.8 mmol/L. Hemoglobin and hematocrit (Hb & Hct) were 15 g/dL and 47%, respectively. Infant’s blood type was A positive, Rh positive with positive Coombs reactivity. Reticulocytes count was 5%.
Infant’s Early Onset Sepsis (EOS) risk was low, it was calculated using the sepsis risk calculator (SRC),7
and he was tested positive for Treponemal Pallidum Antibodies (TPA) with non-reactive RPR.
The infant received 1 mg intramuscular vitamin K as a standard newborn care. Due to the significant amount of bright bloody meconium, abdominal radiograph was ordered and showed no obstructive gas patterns, no pneumatosis, and no concerns for volvulus.
Hb & Hct were repeated and were stable: 15.7 g/dL and 46.1%, respectively. Apt test,5
which resulted at 12 HOL confirmed that the blood in the infant’s stool was maternal which indicates swallowed maternal blood. At 20 HOL, serum bilirubin was 9.0 mg/dL, which was a high-intermediate level per American Academy of Pediatrics (AAP),8
and phototherapy management was indicated and initiated.
For the first 24 HOL, infant had two more large episodes of bloody meconium filling two diapers like the one shown in , and he had no emesis. He urinated four times, and he continued to be well appearing with unchanged PE and stable vital signs. He was exclusively breastfed with good latch.
At 38 HOL, infant had a bowel movement consistent with melena.
Bilirubin at 52 HOL was 10.4 mg/dL which is low-intermediate level per AAP.8
Therefore, phototherapy was discontinued and infant was discharged home in a stable condition. He had normal stool color prior to discharge from the hospital.
We presented the case of a large amount of bloody meconium that started shortly after birth and prior to breastfeeding; therefore, milk so protein allergy and blistered maternal nipples were ruled out, also no anal fissure was visualized in the infant’s PE. Neonatal sepsis and infectious enterocolitis can also cause bloody stool in infants.3
A positive maternal GBS, especially when accompanied with prolonged rupture of membranes (ROM), chorioamnionitis, premature GA, and inadequate GBS intrapartum antibiotics prophylaxis (IAP), increases the risk for sepsis.7
The mother’s GBS in our case was positive; she received adequate IAP, and she did not have any associated EOS risk factors. SRC was consistent with low risk for sepsis; therefore, in addition to normal PE, an infectious process that could possibly result in gastrointestinal bleeding was less likely. Another consideration for gastrointestinal bleeding in neonates is malrotation and midgut volvulus.3
Patients commonly present with sudden onset bilious emesis, distended abdomen, and signs of shock caused by bowel necrosis, which can be a later finding.
Although NEC can be associated with perinatal asphyxia and sepsis in term infants,5,13,14 the infant in this case was well appearing with normal exam and unremarkable abdominal radiograph. There were no concerns for perinatal asphyxia or sepsis; therefore, NEC was unlikely in this case. There were no suggestive findings of systemic coagulopathy, which may cause bloody stools.3,9 No maternal or family history of thrombocytopenia and/or coagulation disorders.
While the Apt test5
is useful in distinguishing maternal from fetal blood, limitations exist15,16; it is only useful for determining if the sampled blood is predominantly fetal (>0%) hemoglobin or maternal (<10% fetal hemoglobin). Furthermore, tarry or melena specimens can give false positive results.15,16 Modifications of the Apt test have since been made to increase the sensitivity and specificity of the test.16
While this would be the fastest method to determine if the diagnosis for our infant is swallowed maternal blood, the test took 12 h to result. Therefore, further evaluation was warranted to rule out high risk causes.
Swallowed maternal blood was considered in our infant; however, what was concerning was the significant and frequent amount of bloody meconium that started very shortly after birth.
Healthy newborns deserve to have minimal to no interventions. To accomplish this goal, more depth in neonatal conditions similar to the infant in our case should be introduced and discussed. We hope that the valuable figures in this case will provide reassurance to stop unnecessary workups for the purpose of optimal newborn outcome in the least invasive environment. Furthermore, inventing a rapid Apt test that can be obtained at bedside as a point of care would create an innovation in the neonatology world, especially when PE and vital signs are reassuring.
The benign melena neonatorum from swallowed maternal blood can present as massive amount of bloody meconium as early as 10 min of life. Minimal workup may suffice when the infant is stable, especially if Apt test is expedited.
The authors would like to acknowledge the nursing staff in our Mother-Baby Unit who were vigilant in supervising the infant in this case and saved all the belonged blankets and diapers.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval/patient consent: Signed written informed consent is provided by the legally authorized representative of the infant in this case. The infant’s mother signed a written informed consent form for this case report for anonymized patient information to be published in this article. This process is sufficient in our institution for ethics approval.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Rana Alissa https://orcid.org/0000-0003-1903-7674
1.
O’Neil AM, Homme JL. Evaluation of hematochezia in a two-day-old infant. J Emerg Med
2016; 50(1): 41–43. [PubMed] [Google Scholar]
2.
Maayan-Metzger A, Ghanem N, Mazkereth R, et al.
2004; 89(1): F68–F70. [PMC free article] [PubMed] [Google Scholar]
3.
Patel N, Kay M. Lower gastrointestinal bleeding in children: causes and diagnostic approach. UpToDate, https://www.uptodate.com/contents/lower-gastrointestinal-bleeding-in-children-causes-and-diagnostic-approach, 2020.
4.
Bhanu P, Tolia V. Gastrointestinal bleeding in infants and children. Therapy
2008; 5(4): 465–473. [Google Scholar]
5.
Apt L, Downey WS., Jr.
Melena neonatorum: the swallowed blood syndrome; a simple test for the differentiation of adult and fetal hemoglobin in bloody stools. J Pediatr
1955; 47(1): 6–12. [PubMed] [Google Scholar]
6.
Apgar V. A proposal for a new method of evaluation of the newborn infant. Originally published in July 1953, volume 32, pages 250–259. Anesth Analg
2015; 120(5): 1056–1059. [PubMed] [Google Scholar]
7.
Kuzniewicz MW, Puopolo KM, Fischer A, et al. A quantitative, risk-based approach to the management of neonatal early-onset sepsis.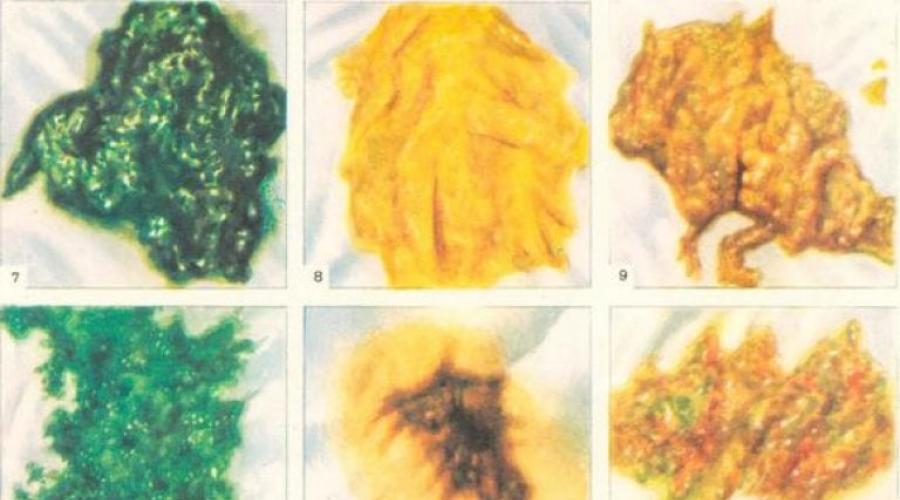
2017; 171(4): 365–371. [PubMed] [Google Scholar]
8.
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics
2004; 114(1): 297–316. [PubMed] [Google Scholar]
9.
Gomella TL, Cunningham MD, Eyal FG, et al. Bloody stool (chapter 49). In: Gomella T, Cunningham M, Eyal FG, et al. (eds) Neonatology: management, procedures, on-call problems, diseases, and drugs. 7th ed.
New York: McGraw Hill, 2013, pp. 351–357. [Google Scholar]
10.
Chu A, Chiu HK. Necrotizing enterocolitis in the full-term infant. Pediatr Ann
2015; 44(10): e237–e242. [PubMed] [Google Scholar]
11.
Al Tawil K, Sumaily H, Ahmed IA, et al. Risk factors, characteristics and outcomes of necrotizing enterocolitis in late preterm and term infants. J Neonatal Perinatal Med
2013; 6(2): 125–130. [PubMed] [Google Scholar]
12.
Sharma R, Hudak ML, Tepas JJ, 3rd, et al. Impact of gestational age on the clinical presentation and surgical outcome of necrotizing enterocolitis.
2006; 26(6): 342–347. [PubMed] [Google Scholar]
13.
Fox TP, Godavitarne C. What really causes necrotising enterocolitis?
ISRN Gastroenterol
2012; 2012: 628317. [PMC free article] [PubMed] [Google Scholar]
14.
Ng S. Necrotizing enterocolitis in the full-term neonate. J Paediatr Child Health
2001; 37(1): 1–4. [PubMed] [Google Scholar]
15.
Kim CR, Park IK. Direction of Apt test modification: sensitivity and simplicity. J Pediatr
2015; 166(3): 781. [PubMed] [Google Scholar]
16.
Liu N, Wu AH, Wong SS. Improved quantitative Apt test for detecting fetal hemoglobin in bloody stools of newborns. Clin Chem
1993; 39(11 Pt 1): 2326–2329. [PubMed] [Google Scholar]
Articles from SAGE Open Medical Case Reports are provided here courtesy of SAGE Publications
Baby Poo Guide- Types, Colours and What they Mean
Home
/
Baby
/
Baby Health and Illnesses
/
Baby poo — a visual guide
Baby By Month
1 1
2 2
3 3
4 4
5 5
6 6
7 7
8 8
9 9
10 10
11 11
12 12
13 13
14 14
15 15
16 16
17 17
18 18
19 19
20 20
21 21
22 22
23 23
Baby
-
Expand pages
Newborn Baby Care -
Expand pages
Baby Skincare -
Expand pages
Baby Health and Illnesses -
Expand pages
Breastfeeding -
Expand pages
Monthly Baby Development -
Expand pages
Baby milestones -
Expand pages
Sleep -
Expand pages
Teething -
Expand pages
Weaning -
Expand pages
Games and activities -
Expand pages
Potty training -
Expand pages
Your childcare options -
Expand pages
Child behaviour -
Expand pages
Food & nutrition -
Expand pages
Baby clothing -
Find your nearest baby photographer -
Expand pages
Baby classes
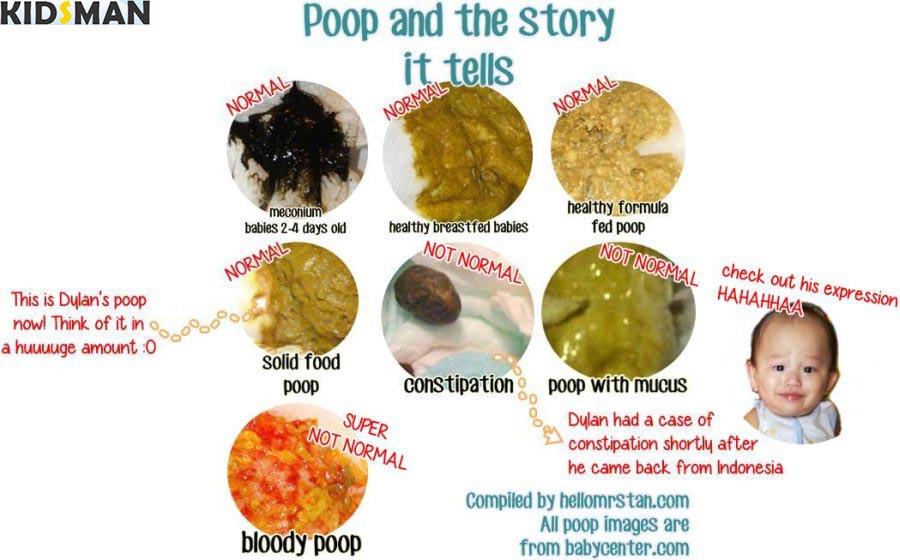
A photographic guide — Types of Baby Poop & What They Mean
Here you’ll find your ultimate baby poo colour chart to help you better understand your baby’s poo and what it means.
Meconium
Your baby’s first poos are called meconium. They are a dark, greenish black colour and very sticky, almost like tar. Meconium is made from substance your baby ingested in the womb, such as amniotic fluid, mucus, skin cells and lanugo (the fine hair
that covered your baby’s body). Meconium doesn’t smell and only lasts for a few days.
Breast-fed poo
This is a mustardy, yellow colour, loose, with a grainy or seedy texture. Because it is soft and runny, it can sometimes be mistaken for diarrhoea. Breastfed poo has a sweet smell.
Bottle-fed poo
It is harder for a baby to digest formula than breast milk so the poo of a bottle-fed baby is bulkier than that of a breastfed baby. It’s likely to be a pale yellow or yellowish brown colour with a smell that’s more like your own poo.
Solid food poo
Once your baby starts on solids his poo will change and become larger and thicker, more like an adult’s
poo.
Diarrhoea
Diarrhoea poo can be yellow, green or brown
in colour and is very watery and runny. It can seep or even explode out of the nappy. Often a result of an infection or allergy, it can lead to dehydration if it continues for 24 hours or if your baby is vomiting as well, is feverish, passing blood
or has mucus in the poo, or has abdominal pain you should seek urgent medical advice.
Constipation
Hard poo that is difficult to pass and look like rabbit droppings are a sign of constipation.
Your baby may strain, cry and go red in the face while he tries to poo. If there is any sign of blood in the poo you should contact your GP or health visitor.
Poo with blood
Blood in the poo is usually a symptom of constipation.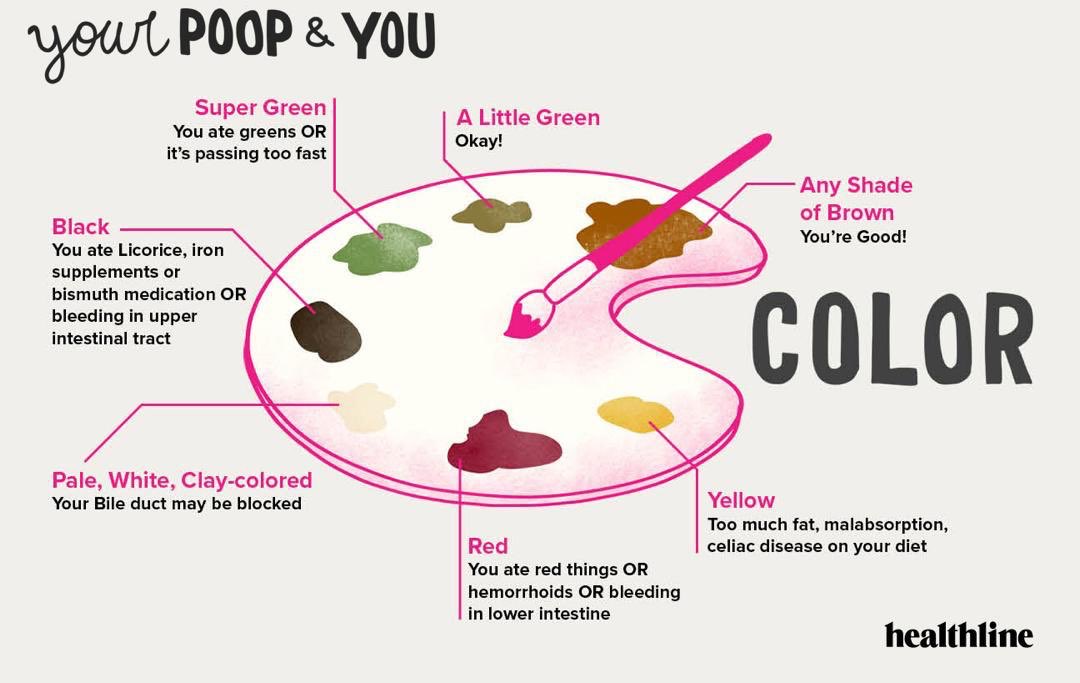
Green poo
This can be a sign that a breastfed baby is not latched on properly so that he’s drinking a lot of the watery milk at the beginning of the feed and is not getting enough of the fat-rich milk at the end of the feed. Ask your healthcare professional
to check your latch and make sure your baby empties one breast before starting on the second one.
Poo with mucus
Poo streaked with slimey mucus can be a sign of an infection or allergy. If it’s accompanied by other symptoms or lasts for more than two days seek medical advice.
Bloody baby poo
It’s important to note that if you notice blood in your little one’s poo, whilst this can be a symptom of constipation, you should call your
health visitor or GP.
MORE ABOUT CREATING A HEALTHY HOME FOR BABY
Your baby’s poo can be a good indicator of how they are feeding and whether they are well.
Are you a member of the Emma’s Diary Parenting Club? Join today to access lots of freebies for your new baby plus member-only discounts and offers!
THE LATEST HOT TOPICS
Is my baby getting enough vitamin D?
Find out everything you need to know…
Read more
Your guide to breastfeeding & expressing
Here’s everything you need to know…
Read more
Your baby’s month by month development
Here’s what to expect at every age…
Read more
JUST FOR YOU
An age-by-age guide to baby sleep
Discover how much your little one should be getting…
Read more
Lactose intolerance in babies
What is it? What causes it? Does my baby have it?
Read more
Signs your baby is ready for solid food
Tips and advice you may find useful.
Read more
Emma’s Quick Links
❰Mucus in Feces❱ in Adults — Causes and Treatments
Mucus in the stool may occur due to physiological causes. After all, the production of a small amount of mucus into the intestinal lumen occurs constantly and its traces, indeed, can sometimes be seen in the feces.
But most often visible impurities of mucus in the feces of an adult can indicate such pathological conditions as:
- colitis
- colon polyp
- colon cancer
- diverticular disease of the colon
- dysbacteriosis
- irritable bowel syndrome
- as well as disorders of absorption processes in the lumen of the colon
Mucus in the feces is a possible symptom of a fairly wide list of diseases. A proctologist will help to identify the cause of the presence of mucus in the feces.
You can make an appointment with a proctologist on our website.
Appointment
Why mucus appears in the stool
When the amount of mucus increases, it is often associated with various pathologies. Certain disorders can develop into chronic ones, which is considered a serious threat. Most often, mucus in the stool is a symptom of an inflammatory process. For example, if the substance is slippery and diarrhea, the likelihood of an intestinal infection is high. The appearance of blood in the stool and pain in the abdomen indicate the risk of Crohn’s disease, ulcerative colitis, and even cancer.
Clear mucus stool possible as a side effect of certain drugs and dietary products. For example, NSAIDs, flatulence medications, smoking, and even drinking coffee increase mucus. If you exclude something from this list, you can normalize the concentration of the substance.
What diseases cause mucus in the stool
Jelly-like mucus in the stool can indicate:
- irritable bowel syndrome. The functioning of the intestine is impaired in the absence of pathological formations.
Symptoms of a bowel problem are alternating constipation and diarrhea. The presence of mucus in the feces is typical for this disease
- Crohn’s disease. The inflammatory process is chronic, often difficult, and acts as a catalyst for the appearance of malignant tumors. Lesion from oral cavity to rectum. In most cases there is clear mucus in the stool
- ulcerative colitis. It causes the appearance of ulcers on the mucous membrane. Due to the fact that they bleed, rot, red mucus may appear in the stool. Symptoms also include abdominal cramps, bloating
- proctitis. Inflammation in the rectum. A characteristic sign is white mucus in the stool in an adult
- allergic colitis. Peculiar to children and manifests itself as a reaction to cow’s milk
- oncology of the rectum or colon. The key sign is the presence of blood in the stool. But, feces with white mucus are also possible
- food poisoning. In rare cases, it is accompanied by blood and copious amounts of mucus.
Often things go back to normal after a few days, but if it lasts longer, see a doctor
- membranous colitis. In this case, yellow mucus appears in the stool in an adult
This is only a small part of the diseases accompanied by mucus in the stool. Sometimes these symptoms are associated with temporary indigestion. Jelly-like mucus in the stool in an adult is considered normal, but if we are talking about the minimum amount and transparency. It is best to undergo diagnostics at Mediland Medical Center in order to detect the disease in a timely manner.
When to see a doctor
If an adult has excessively large amounts of stool with mucus, it is easier to say mucus instead of regular stool, this is a signal of a serious illness. You need to see a doctor. Other symptoms are also possible:
- there is blood in the stool
- yellow mucus in feces — purulent or bacterial process, also one of the signs of hemorrhoids and polyps
- frequent diarrhea
- spasms, abdominal pains
Mucus with feces with any signs should be regarded as the need to visit a doctor for a complete examination.
White stool is one sign of serious diseases: hepatitis, liver tumors, problems with the pancreas. Stercobilin affects the color of feces, if it falls or decreases, the development of pathologies dangerous to the human body may begin.
Diagnostic methods for the appearance of feces with mucus
Doctors of Mediland Medical Center for maximum accuracy in diagnosing thick mucus in the feces use different approaches:
- detailed blood test
- coprogram
- stool examination for infections, occult blood
- colonoscopy — examination of the mucous membrane of the rectum and colon with a colonoscope
- sigmoidoscopy — diagnostics of the rectum and sigmoid colon
- examination of the stomach, esophagus
- video capsule endoscopy is prescribed for the study of the digestive tract.
A capsule with mini-cameras is used, the patient swallows it, doctors get the opportunity to assess the patient’s condition
- referral for CT and MRI
If mucus is found in the stool, for treatment, you need to make an appointment with a doctor. With early diagnosis, the likelihood of a quick recovery and a decrease in the risk of complications of the disease increases. Mediland MC offers basic instrumental and laboratory diagnostic approaches. In addition, the patient consults with advanced doctors.
What to do
The appearance of an admixture of mucus in the stool in an adult requires a total examination of the colon by colonoscopy. It is a visual examination of all parts of the large intestine that will allow not to miss the initial stages of dangerous diseases.
At Mediland Medical Center, colonoscopy is performed under intravenous anesthesia and does not cause any discomfort to the patient. Research data can be recorded on a computer hard drive and, if necessary, handed out to the patient.
Before signing up for such an examination (colonoscopy), it would be rational to consult a proctologist. The specialist will select the correct examination algorithm, depending on the specific situation, if necessary, appoint consultations of doctors of related specialties and draw up a treatment program based on the data received.
What not to do
Do not under any circumstances use information obtained from the Internet to form your own idea about the cause of health complaints and methods for their elimination.
Do not take advice from friends, neighbors and acquaintances on how to get rid of the problem, based on their positive experience. Remember that mucus in the feces can be a symptom of various diseases, and what gave an excellent result in the case of your «adviser» can have a completely opposite effect on your body.
It should be remembered that self-treatment (including, at first glance, successful), the patient can level the symptoms of the disease, but not cure the disease.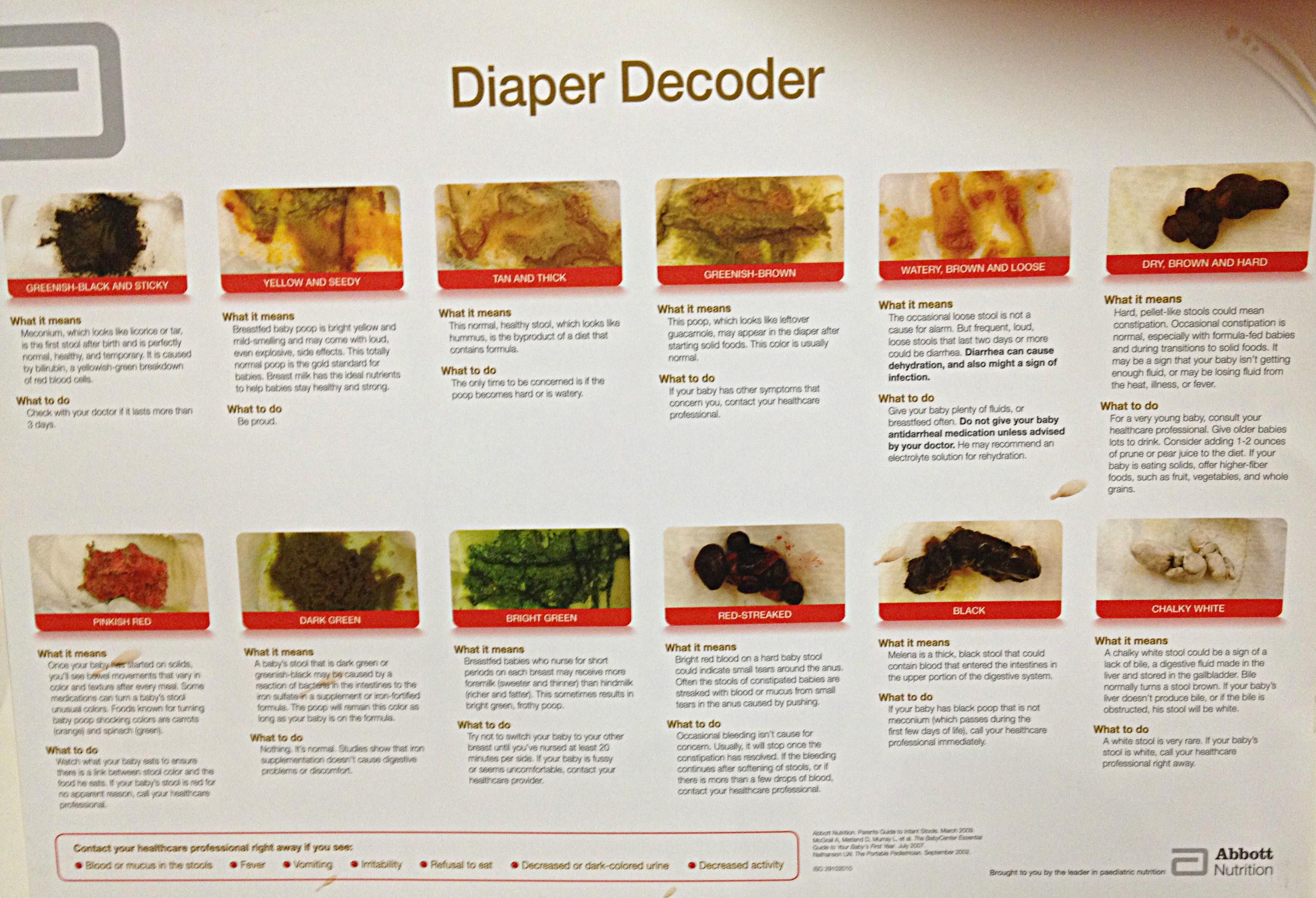
Do not be afraid of a visit to the doctor and diagnostic procedures. Qualified proctologists of Mediland Medical Center perform all procedures correctly, without causing any physical or moral suffering to the patient.
It is important to remember — the loss of time in matters of diagnosis and treatment often turns simple cases of diseases into big health problems! Proctologist, Surgeon, Phlebologist PhD, Associate Professor, is a member of ESCP, IPS
Important to know
What to do
The appearance of an admixture of mucus in the feces in an adult requires a total examination of the colon by colonoscopy. It is a visual examination of all parts of the large intestine that will allow not to miss the initial stages of dangerous diseases.
At Mediland Medical Center, colonoscopy is performed under intravenous anesthesia and does not cause any discomfort to the patient.
Before signing up for such an examination (colonoscopy), it would be rational to consult a proctologist. The specialist will select the correct examination algorithm, depending on the specific situation, if necessary, appoint consultations of doctors of related specialties and draw up a treatment program based on the data received.
What not to do
Under no circumstances should you use information obtained from the Internet to form your own idea of the cause of complaints and methods for their elimination.
Do not take advice from friends, neighbors and acquaintances on how to get rid of the problem, based on their positive experience. Remember that mucus in the feces can be a symptom of various diseases, and what gave an excellent result in the case of your «adviser» can have a completely opposite effect on your body.
It should be remembered that self-treatment (including, at first glance, successful), the patient can level the symptoms of the disease, but not cure the disease.
Do not be afraid of a visit to the doctor and diagnostic procedures. Qualified proctologists of Mediland Medical Center perform all procedures correctly, without causing any physical or moral suffering to the patient.
It is important to remember — the loss of time in matters of diagnosis and treatment often turns simple cases of diseases into big health problems!
Appointment
Like it? Share with friends:
Diarrhea in a cat (cat) — what to do, how to treat at home
Diarrhea is a digestive disorder, which is expressed in a change in the consistency of feces to a liquid or watery form and an increase in the frequency of the urge to defecate.
Many owners do not think this problem is serious, although in fact it requires special attention from the owner and specialist.
It is also worth noting that diarrhea is not an independent disease, but only a consequence of existing pathologies.
Symptoms of diarrhea in cats
The main and only symptom of diarrhea is frequent and loose stools, which is repeated more than 3 times a day. In addition, a cat or cat sometimes has fecal incontinence and the presence of blood streaks in it. Flatulence and gas emission are also possible.
Let’s single out the characteristic symptoms of diarrhea:
- frequent defecation;
- the consistency of the stool changes — it becomes frothy, watery, has impurities of blood streaks, mucus;
- the hue may change — normal feces are brown, and with diarrhea there is a lighter or greenish stool;
- the smell may be putrid, sour, offensive.
In addition to diarrhea, the cat may lose its appetite. She becomes lethargic, lies more, hides in secluded places, loses weight. Sometimes there is an increase or decrease in body temperature.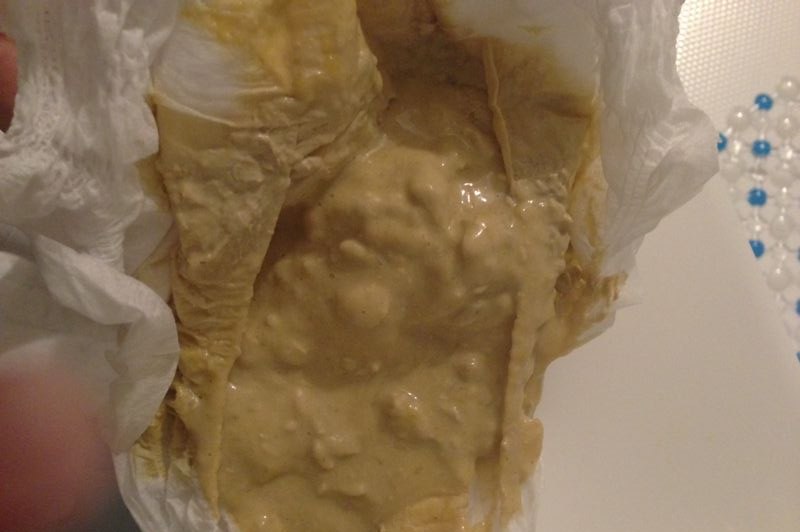
In some cases, vomiting occurs along with diarrhea. Then dehydration intensifies and urgent measures must be taken to treat the animal. First of all, it is necessary to replenish the lost fluid, as well as stop diarrhea and vomiting.
Causes of diarrhea in cats
Diarrhea can be caused by several causes at once. We have divided them into separate groups to make it easier for you to understand what causes diarrhea in cats.
1) Food reasons
- Changing the usual diet — switching from one food to another and vice versa, changing water, unbalanced nutrition.
It is necessary that the transition to a new diet in a cat is carried out gradually. To do this, you must reduce the amount of familiar food and increase the amount of new. If this rule is neglected, then the microflora and enzymes of the gastrointestinal tract will not be able to abruptly adjust to the new mode of operation and will “go on strike” in the form of diarrhea.
- Improper feeding — the inclusion in the diet of foods that cause indigestion.
- Overfeeding — overfeeding affects digestive disorders, but regurgitation and vomiting are most often involved. Especially when the cat eats quickly, while swallowing air.
- Food poisoning is the body’s reaction to eating poor-quality, spoiled food.
We boldly include those who like to eat waste from the trash and those who love to gnaw flowers into the risk group. When poisoned, the cat’s body tries its best to get rid of toxins that threaten its safety, as spoiled food causes intoxication.
- Food allergy — here we usually present redness of the skin, itching, watery eyes. Diarrhea is also one of the symptoms of allergies.
This reaction does not necessarily make itself felt immediately after the first intake of a new food. Manifestations can intensify over time — with each new hit of the «aggressor» in the cat’s body.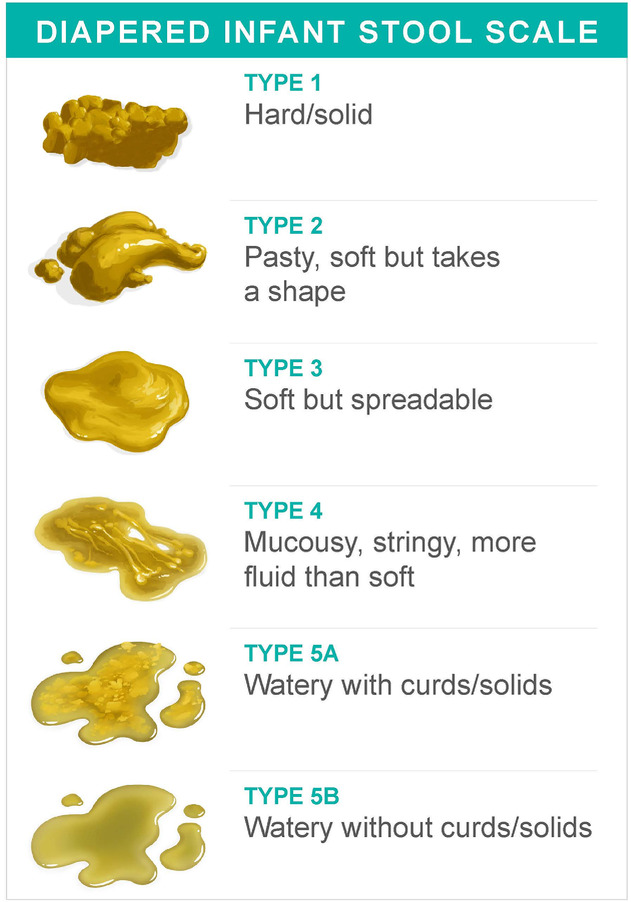
- Intolerance, intestinal sensitivity to certain food components.
What is the difference between intolerance and allergy? An allergy is a feature of the immune system, its pathological reaction to something that has entered the body. Intolerance is the inability of enzymes to digest foods that contain a particular ingredient, such as gluten. In this case, the gastrointestinal tract reacts to the problem with regular vomiting or diarrhea.
2) Contagious causes of diarrhea in a cat
- Parasitic infestation (helminthiasis) — these are helminths or worms, in simple terms.
To prevent their occurrence and spread, it is recommended to regularly deworm pets. If a significant number of parasites live in the cat’s body, they cause intestinal irritation and malfunctions, such as diarrhea.
- Infectious diseases of the gastrointestinal tract:
- Bacterial (eg salmonellosis, colibacillosis).
Transmission of pathogens is possible through feed, water and excretions of sick animals. Symptoms may not appear for a long time, and then triggered by severe stress or other comorbidities.
- Protozoan infections (cryptosporodiosis, trichomoniasis, toxoplasmosis).
From the point of view of the symptoms of the gastrointestinal tract, we distinguish giardiasis and trichomoniasis. They are easily transmitted through the faeces of sick cats, and in both cases, diarrhea is the leading symptom.
- Viral (viral leukemia, panleukopenia).
Coronavirus gastroenteritis, viral leukemia, panleukopenia, viral immunodeficiency should be noted among viral infections. Infection occurs in most cases by contact — through the discharge, feces of sick animals. Diseases are quite severe and can lead to death. However, some of them are preventable by vaccination.
3) Pathologies associated with the digestive system:
- Pancreatitis — inflammation of the pancreas.
When it spreads to the intestines, diarrhea is observed.
- Diseases of the kidneys. Diarrhea in this case is an unobvious but common symptom. It manifests itself most often in the later stages of the disease.
- Pathology of the liver and biliary tract. The liver is a fairly multifunctional organ, and the general condition and quality of life of the animal depends on its work. The gastrointestinal tract also reacts to changes in the liver, so one of the symptoms of its damage may be diarrhea and a change in the color of the stool in a cat.
- IBD — inflammatory bowel disease. This is the name of a group of symptoms (vomiting, diarrhea, change in appetite), which are persistently repeated and not amenable to standard therapy. This is a complex diagnosis that is often made after all other possible problems have been ruled out.
- Metabolic disorders, including diabetes mellitus. Most often occurs in old age. In case of violations of metabolic processes, the work of internal organs changes, and secondary infections also appear.
- Oncological diseases — neoplasms affecting the internal organs of the cat, most often its digestive system and kidneys. May be accompanied by various clinical signs.
4) Other causes:
- Certain medications, such as antibiotics and NSAIDs (non-steroidal anti-inflammatory drugs).
Medicines can disturb the microflora of the digestive tract, thereby causing diarrhea.
- Heat stroke.
This is a dangerous condition in which the body overheats and the animal becomes restless. With sunstroke, there may be vomiting and convulsions, diarrhea is possible, and in some cases there is loss of consciousness.
- Stress is a negative reaction to a move, a long trip, a new pet in the house, etc.
Each such situation is capable of provoking stress. In addition to diarrhea, it is possible to observe in a cat excessive licking of wool and skin, unusual behavior, active molting, involuntary urination, loss of appetite.
- Hairballs in stomach
If hair is found in the intestines of a cat, it can irritate the mucous membranes and villi of the gastrointestinal tract, thereby causing diarrhea. But more often in this case there is constipation, rather than diarrhea.
- Pregnancy and postpartum period.
New food, food from the table of different origin, the presence of secondary diseases and infections, overeating, helminthiasis, hormonal changes — all this can cause diarrhea in a pregnant cat. However, the appearance of diarrhea a couple of days before childbirth is considered the norm.
- Foreign objects in the digestive tract
If there is intestinal obstruction, vomiting and no stools occur. But blockage can be caused by different reasons, which means that the appearance of diarrhea can also be one of the symptoms.
Diarrhea in cats without complications
If you notice periodic diarrhea in your pet, and at the same time he does not lose weight, appetite, looks active — this is still a reason to visit the veterinary clinic.
To understand what to do if the cat has diarrhea, you need to assess the patient’s well-being. If the animal is deteriorating or has other symptoms, do not treat it yourself.
If the diarrhea is due to a sudden change in diet, the cat should be on a fast diet for several hours, but the water should be left.
Important : Felines should not be without food for a long time. Prolonged hunger has a very detrimental effect on their liver, and then on the whole body as a whole. If the cat does not eat for more than 12 hours, you should be wary and show the pet to the doctor.
Diarrhea with water
This phenomenon in cats is one-time. But it is worth considering that this symptom may indicate the onset of the disease. With a single episode, the cat needs to increase its water intake.
Loose stools with blood or mucus
The large intestine protects itself, its walls, by secreting a large amount of mucus. If a cat has diarrhea with blood, this indicates a slight lesion of the capillaries of the large intestine. Then you can suspect helminthic invasion, food poisoning, irritation of the wall of the large intestine.
If there is blood in the stool, and it can be scarlet, cherry, brown, black or streaked, then it is necessary to exclude or confirm the presence of a foreign body in the stomach or intestines, as well as the presence of neoplasms or viral infections. This condition is characterized as acute, so it is urgent to take the cat to the clinic.
Diarrhea and vomiting in cats
If the cat vomits and diarrhea is observed, then we can assume poisoning, neoplasms, a foreign body in the gastrointestinal tract, a viral infection, pancreatitis, etc.
Color of diarrhea
The color of the stool can be used to determine the causes of diarrhea. Let’s designate them.
-
Black
Characteristic of a high level of iron in the body of a cat (for example, due to the consumption of raw meat in large quantities).
Black-red color indicates bleeding in the gastrointestinal tract. The reasons may be poisoning, neoplasms, the presence of foreign bodies, etc. In this state, help is provided to the cat immediately.
-
Yellow
Yellow diarrhea indicates a violation of intestinal motility, improper digestion, problems with the bile ducts.
Normally unformed yellow stool occurs only in kittens on a milk diet. In an adult cat, diarrhea of this color indicates a violation of the liver.
-
Green
This diarrhea warns you that your cat has eaten spoiled foods that have caused putrefaction and fermentation.:max_bytes(150000):strip_icc()/healthy-and-unhealthy-stool-89211-color-V1-9cef9502a0a5433994307575289f34c7.png)
The pathological causes of the green color of feces include: parasitic infections, a sharp change in food, increased intestinal motility, acute inflammation of the gastrointestinal tract.
-
White
He talks about problems with the biliary tract, and also with the liver or pancreas.
Treatment of diarrhea in cats and cats
Often owners have a question — how to treat diarrhea in a cat. Let’s talk briefly.
Therapeutic deworming is indicated for helminthic invasion. Now drugs are actively used in a variety of dosage forms (tablets, suspensions, drops on the withers) based on milbemycin (Milbemax), praziquantel and fenbendazole (Kaniquantel), praziquantel and pyrantel (Drontal).
When it comes to pathologies of the liver and kidneys, therapy regimens corresponding to a particular disease are prescribed. In addition, supportive therapy is carried out.:max_bytes(150000):strip_icc()/advice-about-bright-red-blood-in-stool-796937-v3-004a17fa66384362918ed65f63233acd.png)
In intestinal diseases, there is pain in the abdominal cavity. In such cases, antispasmodic drugs (Spasmalgon, Papaverine) may be prescribed.
With profuse diarrhea, as well as in case of vomiting, there is a risk of dehydration. Then infusion therapy (droppers) is used — intravenous administration of solutions (Sodium chloride, Ringer’s solution, Ionosteril, Sterofundin).
In terms of the duration of therapy, sometimes the treatment takes only a couple of days, while in other cases it is possible to achieve a stable effect only after a few weeks of treatment.
Therefore, if the cause of the disease is established correctly, then the treatment of diarrhea in a cat leads to recovery. To do this, the doctor needs to collect a complete history:
- presence or absence of annual vaccination;
- taking anthelmintic drugs and the frequency of their use;
- type of food or natural food composition;
- application of vitamins;
- the possibility of using inedible products: leaves or parts of plants, foreign objects, tablets that could be freely available for the animal.
The doctor conducts a complete examination of the cat, measures its body temperature, determines the degree of dehydration, the condition of the mucous membranes, pain in the abdomen. After that, the clinic will take blood tests, do an ultrasound of the abdominal cavity, and possibly collect tests for infections accompanied by intestinal symptoms.
At home
To properly treat diarrhea, you need to understand the underlying cause. It is very important to know that the dosage of drugs for animals is different from that for humans. They can not be dosed for a cat, as for a baby.
Important : We do not recommend self-medication, because only a specialist can answer the question of what to give a cat for diarrhea.
At the same time, according to the doctor’s prescription at home, you can independently give your pet adsorbents — Smecta, Regidron, Polysorb, Enterosgel, activated carbon. These are the most common remedies for stool disorders.
Fortiflora for cats, Lactobifadol, Evitalia Vet, Vetom help restore intestinal microflora. With pain in the abdominal cavity, you can give the animal antispasmodic drugs prescribed by prescription, for example, Drotaverine, Papaverine.
Veterinary help
You have already understood that with all types of diarrhea, you need to go to the veterinary clinic. We also found out what diseases and conditions diarrhea can accompany and took into account that therapeutic treatment will be different for different pathologies. Therefore, the owner must clearly record the symptoms of his pet in order to help the doctor to make a complete clinical picture.
A veterinarian is required if the cat:
- is vomiting;
- is noted to refuse food and water, she lies a lot and does not want to walk;
- the temperature rose above 39.
0 degrees;
- the frequency of going to the stool tray is more than 4-5 times a day.
It is essential to contact the clinic if:
- the kitten is less than 1 year old;
- there is a temperature;
- the animal does not eat or drink;
- the color of the stool has changed, there is blood, mucus in the feces;
- diarrhea is accompanied by vomiting;
- observed weight loss;
- marked convulsions;
- diarrhea lasts more than two days;
- reduced activity;
- the frequency of defecation is increased more than 5 times a day.
Medications
Now let’s name the main antidiarrheal drugs, answering the question, what else can be given to a cat for diarrhea:
- Loperamide — Use only after consulting a veterinarian. Not suitable for independent use. It has a strong effect on intestinal motility, to the extent that after acute diarrhea, constipation can occur.
- Smecta is an adsorbent that stops diarrhea well. It can be used on kittens and pregnant cats.
- Enterosgel is an adsorbent that removes toxins and allergens from the body. It is used when poisoning is suspected. Can also be given to kittens and pregnant women.
- Enterofuril is an antimicrobial drug. Suppresses the growth of pathogenic microflora that can cause diarrhea in a cat.
Do’s and Don’ts for Diarrhea in Cats
If your pet has diarrhea, there are some important guidelines to follow. Let’s list them:
- Give food warm. So it will be more pleasant to smell and easier to digest.
- Boil or steam natural foods, as raw, fried foods irritate the mucous membranes. To facilitate digestion, food is crushed in a blender or mashed.
- Give your pet plenty of clean water to replenish moisture loss.
- When feeding industrial products, transfer the animal to treatment lines to restore the gastrointestinal tract (Hill’s Prescription Diet I / D, Royal Canin Gastro Intestinal moderate calorie, Purina EN, Farmina Vet Life Cat Gastrointestinal).
- Reduce portions, but feed frequently — every 2 hours, 1-2 teaspoons.
What to do is strictly prohibited:
- Give raw meat products, vegetables, sour milk, fatty meat and fish, lard, milk, vegetable and butter, bread, sweets, etc. from the table.
- Self-administer medicines without knowing their exact effect and proper result.
- For a long time to withstand the cat’s hunger, rages of the desire to «cleanse» the gastrointestinal tract.
Cat Diarrhea Diet
Feeding during diarrhea depends on the cat’s diet. Therefore, we will answer the popular question: what to feed a cat with diarrhea.
If she consumes industrial feed, then a diet based on therapeutic diets is necessary. This is an easier option for digestion. If the cat eats only natural food, then it is advisable to choose one type of lean protein (chicken, turkey, rabbit), one type of carbohydrates (cereals, vegetables), and you can also offer him baby food based on meat tastes.
Spicy, fried, salty, dried, raw, dairy should not be given! It is also required to exclude food from the table and any goodies.
During a flare-up, it is better to remove dry food completely and give only wet food. If the cat does not tolerate it well, you need to choose a diet for animals with sensitive digestion.
For diseases of the gastrointestinal tract, the Gastrointestinal range of feeds prescribed by doctor’s prescription is well suited. They help support digestion and stool, and keep your pet at a normal weight.
Prevention
The basis for the prevention of diarrhea in cats is to feed a commercial balanced diet with a suitable expiration date. You also need to follow the storage rules: dry food should be in a closed pack, and moist after opening it is better to transfer it to a glass container and put it in the refrigerator.
If the animal is on a natural diet, then it must be made balanced. To do this, you can seek the advice of a veterinarian.

 Symptoms of a bowel problem are alternating constipation and diarrhea. The presence of mucus in the feces is typical for this disease
Symptoms of a bowel problem are alternating constipation and diarrhea. The presence of mucus in the feces is typical for this disease  Often things go back to normal after a few days, but if it lasts longer, see a doctor
Often things go back to normal after a few days, but if it lasts longer, see a doctor  A capsule with mini-cameras is used, the patient swallows it, doctors get the opportunity to assess the patient’s condition
A capsule with mini-cameras is used, the patient swallows it, doctors get the opportunity to assess the patient’s condition 
 When it spreads to the intestines, diarrhea is observed.
When it spreads to the intestines, diarrhea is observed. 

 0 degrees;
0 degrees;