Normal formula fed baby poop pictures: Baby poop guide: 11 types of baby poop | Video
Posted onMilk allergy and baby poop: Pictures, symptoms, and treatment
Baby poop can vary greatly. If poop is more watery and frequent than usual and the baby has other symptoms, such as vomiting or refusing to feed, a parent or caregiver may need to consult a doctor. A cow’s milk allergy may be the cause.
Cow’s milk allergy is the most common food allergy in infants. It affects up to 3% of babies in developed countries by the time they turn 1 year of age.
This article discusses milk allergy in babies, how it affects their poop, other symptoms, and how to manage it.
Typical baby poop varies in appearance according to what the baby eats and their age.
When babies are newborn, their poop is thick and black. This is called meconium, which consists of amniotic fluid, skin cells, and other substances the fetus swallowed while in the uterus.
After the first few days, a baby’s poop will transition. The transitional stool will be more of a yellowish-green color and not as thick as meconium.
Once the baby is a few days older, their poop will depend largely on whether they drink breastmilk or formula.
A typical poop from a breastfed baby is usually yellow, green, or brown and seedy. Their stool may be quite soft or runny, but that does not necessarily mean they have diarrhea.
Babies who drink breast milk often need more nappy changes than formula-fed babies, as they digest breast milk faster.
A typical poop from a formula-fed baby is often thicker than that of a breast milk-fed baby. It will be yellow or brown and similar to the texture of peanut butter.
After around 6 months, babies begin eating solid foods. At this time, their poop often becomes firmer and the color may reflect what they eat. For example, babies who eat carrots, sweet potatoes, and pumpkin may have orange poop.
Learn more about baby poop color.
The most common sign that a baby is allergic to milk is blood in their stool. A baby’s poop may also become more runny and frequent, similar to diarrhea.
Learn more about blood in a baby’s stool.
A milk allergy, sometimes called a cow’s milk protein allergy, occurs when the baby’s immune system overreacts to milk protein. It generally occurs with cow’s milk, but it can also occur with sheep and goat milk.
Although babies younger than 6 months do not usually eat solid foods, they may react to dairy proteins in formula or breast milk.
When this happens, the baby’s body will produce histamines to “attack” the milk. It is different from lactose intolerance, which occurs when a person can not digest the sugar in the milk, called lactose.
About 80% of children will outgrow the allergy by the time they reach 16 years.
The allergic reaction can cause various symptoms aside from a change in the baby’s stools.
Like other food allergies, symptoms of a cow’s milk allergy can range from mild to severe. These symptoms can include:
- hives or a red, itchy rash — though there may be no redness on darker skin
- upset stomach
- vomiting
- colic
- coughing
- wheezing
- congestion
Symptoms often start within 2 hours of coming into contact with milk but can also be immediate.
Delayed reactions
Most reactions to milk appear soon after a baby comes into contact with milk. However, in some, a reaction can occur more than 20 hours after contact. Doctors call this delayed type hypersensitivity.
Symptoms of these delayed reactions are mainly gastrointestinal. A parent or caregiver may notice:
- changes in stool
- bloody diarrhea
- weight loss
- vomiting
- pale skin
- lethargy
Serious reactions
In rare cases, a baby may have a serious allergic reaction to milk, resulting in anaphylaxis, which can be life threatening.
Symptoms of a serious reaction include:
- difficulty breathing
- swelling of the tongue
- shock
- drop in blood pressure
Infants may also experience nonclassical signs of anaphylaxis, including:
- ear pulling
- tongue thrusting
- fussiness
- increased clinginess to the caregiver
Serious reactions generally occur within minutes of consuming milk or foods containing milk.
If they suspect a milk allergy, caregivers can take a baby to a pediatrician for a diagnosis. The pediatrician may recommend an appointment with an allergist.
An allergist will conduct a medical review and discuss the baby’s symptoms, including when they occur and their severity. They may also ask about the parents’ medical history.
During the exam, the doctor may recommend using a skin prick test. In this test, the doctor makes a scratch with a small milk sample on the skin. They will then wait 15–20 minutes to see if a rash or welt appears. They will likely diagnose the baby with a milk allergy if it does.
However, around half of milk allergies in babies are “nonimmunoglobulin E (IgE)-mediated.” This means they occur from a reaction involving components of the immune system other than IgE antibodies. These allergies typically take longer to present with symptoms, making them difficult to recognize. Skin testing does not help in diagnosis. In these cases, an allergist will recommend excluding milk from the diet and then reintroducing it to see if a reaction occurs.
Learn more about allergy testing.
Unless the baby experiences a severe, life threatening reaction, the best treatment for a milk allergy is to avoid milk and foods containing it.
If the baby drinks formula, a doctor will recommend switching to a soy or dairy-free formula option.
Breastfed babies can react to milk proteins if the person producing breast milk consumes dairy. In these cases, the nursing individual should avoid dairy products.
For children with a food allergy, doctors may advise caregivers to carry an auto-injector containing epinephrine, which treats anaphylactic shock.
Learn about dairy milk substitutes.
At around 6 months, babies begin trying solid foods, although their main source of nutrition remains either formula or breast milk.
When introducing new foods, parents and caregivers should pay attention to food labeling. It is best to avoid all products that contain milk or dairy.
Labels may help people avoid potential exposure, but a person can also benefit from knowing which foods to avoid. Some products that contain dairy include:
- butter
- yogurt
- custard
- pudding
- milk
- some baked goods
- cheese
- cream
- ice cream
If in doubt, a parent and caregiver can talk with a health professional about foods that may cause a reaction in a baby.
A parent or caregiver should contact a doctor immediately if they notice blood in a baby’s poop. This is the most common sign of a milk allergy.
A caregiver may also want to contact a doctor if they notice any unusual digestive symptoms in their baby. A doctor can help diagnose the issue.
Babies with a milk allergy may outgrow it as they get older. About 80% of children will outgrow the allergy when they are 16 years of age.
Children who have high levels of cow’s milk antibodies in their blood are the least likely to outgrow their allergy.
Those who do not outgrow the allergy usually need to avoid milk and dairy products. However, allergy experts suggest that consuming dairy in baked goods may help build up a tolerance. Caregivers should talk about this with an allergist before trying it at home.
Babies can react to milk proteins in formula, breast milk, or solid foods. The most common sign is blood in the stool.
Allergic reactions range from mild to severe. Mild reactions cause symptoms such as changes in the stool and vomiting. A severe reaction can cause difficulty breathing and may be life threatening. In these cases, people should seek immediate emergency help.
Most babies eventually outgrow a milk allergy. Until they do, parents and caregivers should avoid giving them dairy products. They may also need to keep an emergency epinephrine auto-injector in case of accidental exposure and a severe reaction.
Milk allergy and baby poop: Pictures, symptoms, and treatment
Baby poop can vary greatly.
Cow’s milk allergy is the most common food allergy in infants. It affects up to 3% of babies in developed countries by the time they turn 1 year of age.
This article discusses milk allergy in babies, how it affects their poop, other symptoms, and how to manage it.
Typical baby poop varies in appearance according to what the baby eats and their age.
When babies are newborn, their poop is thick and black. This is called meconium, which consists of amniotic fluid, skin cells, and other substances the fetus swallowed while in the uterus.
After the first few days, a baby’s poop will transition. The transitional stool will be more of a yellowish-green color and not as thick as meconium.
Once the baby is a few days older, their poop will depend largely on whether they drink breastmilk or formula.
A typical poop from a breastfed baby is usually yellow, green, or brown and seedy. Their stool may be quite soft or runny, but that does not necessarily mean they have diarrhea.
Babies who drink breast milk often need more nappy changes than formula-fed babies, as they digest breast milk faster.
A typical poop from a formula-fed baby is often thicker than that of a breast milk-fed baby. It will be yellow or brown and similar to the texture of peanut butter.
After around 6 months, babies begin eating solid foods. At this time, their poop often becomes firmer and the color may reflect what they eat. For example, babies who eat carrots, sweet potatoes, and pumpkin may have orange poop.
Learn more about baby poop color.
The most common sign that a baby is allergic to milk is blood in their stool. A baby’s poop may also become more runny and frequent, similar to diarrhea. It may also contain mucus.
Learn more about blood in a baby’s stool.
A milk allergy, sometimes called a cow’s milk protein allergy, occurs when the baby’s immune system overreacts to milk protein.
Although babies younger than 6 months do not usually eat solid foods, they may react to dairy proteins in formula or breast milk.
When this happens, the baby’s body will produce histamines to “attack” the milk. It is different from lactose intolerance, which occurs when a person can not digest the sugar in the milk, called lactose.
About 80% of children will outgrow the allergy by the time they reach 16 years.
The allergic reaction can cause various symptoms aside from a change in the baby’s stools.
Like other food allergies, symptoms of a cow’s milk allergy can range from mild to severe. These symptoms can include:
- hives or a red, itchy rash — though there may be no redness on darker skin
- upset stomach
- vomiting
- colic
- coughing
- wheezing
- congestion
Symptoms often start within 2 hours of coming into contact with milk but can also be immediate.
Delayed reactions
Most reactions to milk appear soon after a baby comes into contact with milk. However, in some, a reaction can occur more than 20 hours after contact. Doctors call this delayed type hypersensitivity.
Symptoms of these delayed reactions are mainly gastrointestinal. A parent or caregiver may notice:
- changes in stool
- bloody diarrhea
- weight loss
- vomiting
- pale skin
- lethargy
Serious reactions
In rare cases, a baby may have a serious allergic reaction to milk, resulting in anaphylaxis, which can be life threatening.
Symptoms of a serious reaction include:
- difficulty breathing
- swelling of the tongue
- shock
- drop in blood pressure
Infants may also experience nonclassical signs of anaphylaxis, including:
- ear pulling
- tongue thrusting
- fussiness
- increased clinginess to the caregiver
Serious reactions generally occur within minutes of consuming milk or foods containing milk.
If they suspect a milk allergy, caregivers can take a baby to a pediatrician for a diagnosis. The pediatrician may recommend an appointment with an allergist.
An allergist will conduct a medical review and discuss the baby’s symptoms, including when they occur and their severity. They may also ask about the parents’ medical history.
During the exam, the doctor may recommend using a skin prick test. In this test, the doctor makes a scratch with a small milk sample on the skin. They will then wait 15–20 minutes to see if a rash or welt appears. They will likely diagnose the baby with a milk allergy if it does.
However, around half of milk allergies in babies are “nonimmunoglobulin E (IgE)-mediated.” This means they occur from a reaction involving components of the immune system other than IgE antibodies. These allergies typically take longer to present with symptoms, making them difficult to recognize. Skin testing does not help in diagnosis. In these cases, an allergist will recommend excluding milk from the diet and then reintroducing it to see if a reaction occurs.
Learn more about allergy testing.
Unless the baby experiences a severe, life threatening reaction, the best treatment for a milk allergy is to avoid milk and foods containing it.
If the baby drinks formula, a doctor will recommend switching to a soy or dairy-free formula option.
Breastfed babies can react to milk proteins if the person producing breast milk consumes dairy. In these cases, the nursing individual should avoid dairy products.
For children with a food allergy, doctors may advise caregivers to carry an auto-injector containing epinephrine, which treats anaphylactic shock.
Learn about dairy milk substitutes.
At around 6 months, babies begin trying solid foods, although their main source of nutrition remains either formula or breast milk.
When introducing new foods, parents and caregivers should pay attention to food labeling. It is best to avoid all products that contain milk or dairy.
Labels may help people avoid potential exposure, but a person can also benefit from knowing which foods to avoid. Some products that contain dairy include:
- butter
- yogurt
- custard
- pudding
- milk
- some baked goods
- cheese
- cream
- ice cream
If in doubt, a parent and caregiver can talk with a health professional about foods that may cause a reaction in a baby.
A parent or caregiver should contact a doctor immediately if they notice blood in a baby’s poop. This is the most common sign of a milk allergy.
A caregiver may also want to contact a doctor if they notice any unusual digestive symptoms in their baby. A doctor can help diagnose the issue.
Babies with a milk allergy may outgrow it as they get older. About 80% of children will outgrow the allergy when they are 16 years of age.
Children who have high levels of cow’s milk antibodies in their blood are the least likely to outgrow their allergy.
Those who do not outgrow the allergy usually need to avoid milk and dairy products. However, allergy experts suggest that consuming dairy in baked goods may help build up a tolerance. Caregivers should talk about this with an allergist before trying it at home.
Babies can react to milk proteins in formula, breast milk, or solid foods. The most common sign is blood in the stool.
Allergic reactions range from mild to severe. Mild reactions cause symptoms such as changes in the stool and vomiting. A severe reaction can cause difficulty breathing and may be life threatening. In these cases, people should seek immediate emergency help.
Most babies eventually outgrow a milk allergy. Until they do, parents and caregivers should avoid giving them dairy products. They may also need to keep an emergency epinephrine auto-injector in case of accidental exposure and a severe reaction.
Children’s stool color: how to understand what is normal and what is not
Zainiddinova Rabiyat Salakhiddinovna
Candidate of Medical Sciences, pediatrician, neonatologist, specialist in vaccine prevention
Stool in healthy children does not always look the same.
— Rabiyat Salakhiddinovna, what are the main differences between the stool of a newborn on breast, artificial and mixed feeding?
— For breastfed babies, when feeding with an adapted formula, and with a combination of these two types of food, a different type of stool is allowed. For example, a breastfed baby (HB) feels comfortable with a stool frequency of up to 5-8 times a day, and this is the norm. On artificial feeding (IV), the baby can empty the intestines up to 1 time per day or even once every 2 days, and this is also a variant of the norm. The color of the baby’s stool is also different: a mushy yellow stool in a baby on breast milk and a darker and more dense, thick stool in a baby on a mixture.
— How does a child’s stool change from birth to a year?
— Immediately after birth, the stool is very dark (black) in color and is not exactly feces, but rather a mixture of desquamated epithelium, bile fragments, amniotic fluid and prenatal hair. It’s called meconium. Such a dense dark stool can last up to 3 days, then a transitional stool appears — lighter, with the possible inclusion of green.
Green stools in infants are due to the high content of bilirubin, which is normal for the first months of life. As a rule, by the end of the first month, the stool acquires a stable, permanent appearance — it is mushy, yellowish, with small whitish patches.
— What color can a child’s chair be?
— Normal stool color can be all shades of orange and brown: mustard yellow, light brown, brown stool in babies is normal.
If the chair does not fit into the range of familiar shades, it is worth taking a closer look at the condition of the baby. Is he too restless — is he not capricious, is his stomach swollen, has the color of his urine changed. Bloodshot, black or light-colored stools in a child are not the norm and a reason to seek medical help as soon as possible.
- Almost black baby stool — this color is typical only for meconium, for the stool of a newborn older than 1 week this shade is atypical.
- Gray stool resembling putty (greasy) — most often these are manifestations of bile outflow disorders, often fermentopathy and, as a result, impaired formation of full-fledged feces.
- Red stool — often a manifestation of changes in the diet (with the introduction of beets, prunes). But it is necessary to clearly differentiate between red stools and stools interspersed with red or bloody.
Checklist: alarming symptoms that should alert parents, require an assessment of the child’s condition and supervision of a pediatrician
- Unusual stool colors
- Unusual inclusions in the stool
- Foam chair
- Fetid chair
- Loose stools with mucus
- Blood streaks in stool
- Watery stool (stool like water)
— Excluding color, how to determine the presence of pathology in babies by stool?
Baby foamy stool
— It can be an indicator of a deficiency of the normal microbiota, when the physiological process of digestion of food with the participation of microflora is disturbed and the stool changes its consistency.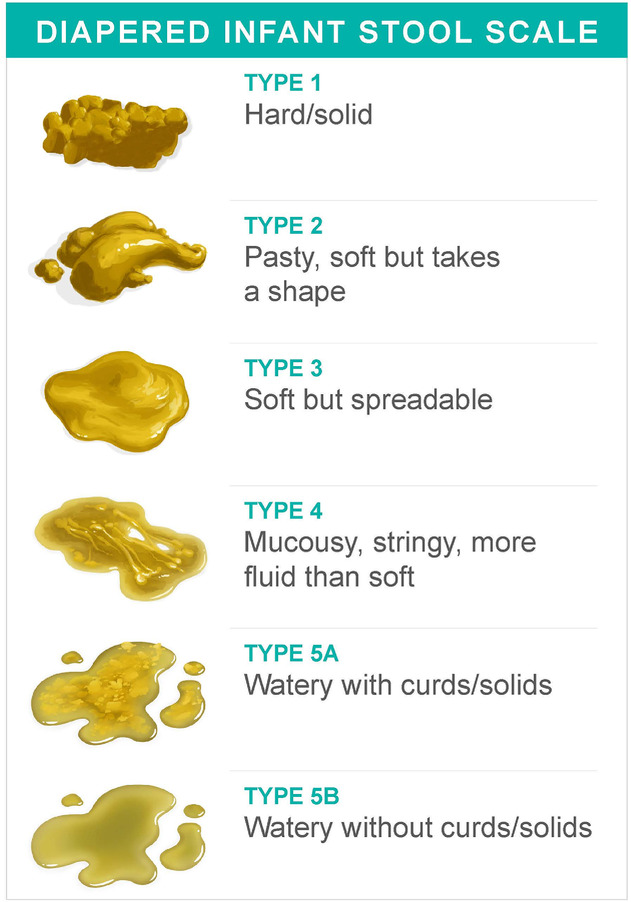
Infant diarrhea
— Diarrhea in children in the first months of life may be caused by an infectious cause or not associated with infections.
Infant constipation
— Constipation can begin to form from the first month of life. The pediatrician should be alerted by such facts as the release of meconium in newborns for more than two days (usually the discharge occurs on the first day).
If a mother notices difficulty in passing stools during the first month of life, it is imperative to bring this to the attention of a pediatrician so as not to miss the symptoms of any serious diseases.
Occult blood in the feces of a child
— There is a medical analysis of feces for occult blood: it shows the presence of microveins of blood that cannot be diagnosed visually.
When assigning a small patient an examination for occult blood in the feces, the doctor looks for possible damage to the integrity of the gastric or intestinal mucosa. In children, due to the tenderness of their mucosa, such damage can be triggered by the listed allergens. Therefore, it is important to exclude a possible risk factor for the development or increase of food allergies.
Stool with mucus and smell
— Speaking of a large amount of mucus in the stool of a baby, you need to remember what mucus is. These are stretching secretions that are the product of the work of the intestinal mucosa: this is how it protects itself from an aggressive acidic or alkaline environment in the process of digesting food. Moreover, a lack of mucus can provoke constipation, although mothers are most often worried about the situation when there is too much mucus in the diaper.
What to look for if there is a lot of clear or white mucus in the feces of a child
For mothers, an isolated abundance of mucus in the feces should not be an alarming symptom, because this in itself is not a full-fledged “red flag”.
Pieces of undigested food in feces
— For many parents, pieces of undigested food in the feces of a child are an alarming sign. They believe that if a child has not digested something, it means that he has some kind of stomach problems and he will not receive enough nutrients.
Causes of small particles of food in the stool
Bad smell
— Unpleasant odor, that is, an odor that is uncharacteristic of normal baby stools, can appear for several reasons.
- A sharp fetid odor of feces is due to an infectious process.
- Unpleasant putrid odor against the background of changes in the consistency of the stool appears with a deficiency of enzymes.
- A different smell and a different structure of feces in one bowel movement will be with constipation, when first a dense fecal stone comes out, and then formed feces.
— Rabiyat Salakhiddinovna, what symptoms may appear along with a change in the color of the stool — what do they talk about and when can they be considered the norm ?.
— As a rule, the variability of shades of the stool itself is acceptable. Dangerous colours: brightly colored blood-streaked, black, greyish-white stools in a child.
When are some of the symptoms associated with a change in stool acceptable?
— What to do to normalize the baby’s stool?
— From a pediatric point of view, it is necessary to mention the presence of surgical diseases in children — those that in pediatrics go under the general name «acute abdomen». This is a whole list of acute surgical conditions at an early age, which are manifested primarily by abdominal pain and unusual behavior of the baby.
Download pdf
Checklist: when parents should not worry, and when to see a doctor
- The child cries very insistently, loudly and piercingly, periods of calm are short, it is not possible to calm him down immediately, or he calms down for a while and begins to sob again; or the condition is accompanied by fever, vomiting, general malaise, stool retention, or uncharacteristic heavy loose stools in infants.
In this case, you need to contact a pediatric surgeon and undergo an abdominal ultrasound to exclude surgical pathology.
- If the disease is caused by the course of a viral infection with abdominal pain syndrome (abdominal pain), then this is a manifestation of the intestinal syndrome on the background of a viral infection. Temperature, colic, flatulence and general malaise are allowed here. Despite the fact that the child’s condition is significantly normalized after taking antipyretic drugs, in any case, it requires examination and control of a pediatrician.
- Knowing about allergic reactions to certain types of foods, the children’s diet is expanded gradually. If a child has mild symptoms such as a change in stool patterns or signs of discomfort such as a single bout of vomiting after taking a new product, then the product may have been introduced early and should be postponed for the time being. Parents need to observe the condition of the child, it is not necessary to immediately consult a doctor.
- During the period of teething, the baby is disturbed by temperature, colic, flatulence, frequent bouts of crying. In this case, the usual stool may change — a stool appears with an abundance of mucus, but without a fetid odor and foam impurities. And this is a situation that is quite acceptable by age, which can be observed by parents and does not require immediate contact with a pediatrician.
Checklist: color and consistency of stool in infants, norm and deviations
Every time, taking off the diaper, willy-nilly, the mother examines its contents. Of course, children’s health is manifested by many symptoms, and children’s stool can also serve as a marker of normal digestion. However, it must be remembered that the characteristics of the stool are extremely variable, they cannot always be the same, and this does not indicate the presence of pathology in the child. But if the baby’s stool has not been formed for several days or weeks, retains an unusual uncharacteristic smell, or has pronounced deviations from generally accepted norms, then it is recommended to consult a pediatrician.
* Breast milk is the best food for babies. WHO recommends exclusive breastfeeding for the first 6 months of a child’s life and continued breastfeeding after complementary foods are introduced until the age of 2 years. Before introducing new products into the baby’s diet, you should consult with a specialist. The material is for informational purposes and cannot replace the advice of a healthcare professional. For feeding children from birth. The product is certified.
#Baby Digestion
#breast-feeding
#baby formula
#Lure
#popular articles
#what’s in the diaper
See also
Omicron in children: how dangerous it is and how babies get sick up to a year
#Advice for Mom
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
How to properly rock a baby to sleep
#Advice for Mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
Neurologist for a child under one year old: first examination
#Tips for Mom
#Baby Development
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
Calendar of doctor visits during the first year of a child’s life
#Advice for Mom
Kizino Polina Aleksandrovna
pediatrician, perinatal psychologist
First tests and vaccinations: how to prepare yourself and your child
#Advice for Mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
Why DHA, ARA and lutein are added to infant formula
#baby formulas
#Baby development
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
Goat’s milk in children’s nutrition: for or against
#Food
#Tips for mom
#Baby digestion
#breastfeeding
Javier Diaz Castro
professor, lecturer
How to tell if a baby has a food allergy
#allergy
#Tips for mom
#breast-feeding
#baby formula
#lure
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
Digestion in newborns and infants and its features
#Baby Digestion
#breast-feeding
#baby formula
#Lure
#Tips for mom
#Baby Development
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
Principles of successful lactation: checklist for mom
#Tips for Mom
#breastfeeding
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
See all
See all
Goat’s milk in children’s nutrition: for or against
# Lure
# Tips for Mom
# Baby’s digestion
# breastfeeding
Javier Diaz Castro
professor, lecturer
Digestion in newborns and infants and its features
# Baby digestion
# breast-feeding
# infant formula
# Lure
# Tips for Mom
# Baby development
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
Neurologist for a child under one year old: first examination
# Tips for mom
# Baby development
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
Calendar of doctor visits during the first year of a child’s life
# Tips for mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
Principles of successful lactation: checklist for mom
# Tips for mom
# breastfeeding
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
How to properly rock a baby to sleep
# Tips for mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
Why DHA, ARA and lutein are added to infant formula
# infant formula
# Baby development
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
Omicron in children: how dangerous it is and how babies get sick up to a year
# Tips for mom
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
See all
First tests and vaccinations: how to prepare yourself and your child
# Tips for mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
How to tell if a baby has a food allergy
# allergy
# Tips for Mom
# breast-feeding
# infant formula
# lure
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
See all
View all
View all
Chair for newborns | Mamovediya
In the first hours and days of life (2–3 days), a newborn produces the so-called original feces — meconium, which looks like a thick mass of dark olive or dark green color, resembling condensed poppy juice.
Original feces are odorless and the first portions are free from bacteria. Its quantity is approximately equal to 60–90 g. In most cases, the discharge of meconium stops on the 2nd day. It also happens that meconium is excreted for a longer time. Then it can be assumed that the child is not getting enough nutrition.
From the 7-8th day, the normal stool for a newborn begins to form — yellowish-golden in color with a sour smell. It happens 4 to 5 times a day and more often. It may contain impurities of greenery and mucus, as well as white lumps.
If the child is bottle-fed, then the stool is usually more plentiful and homogeneous in consistency. Depending on the amount of the mixture, its color may vary — from light yellow to brown. Its smell is quite strong. The number of bowel movements per day is less than in breastfed children, usually one to two per day.
When formula-feeding, you should carefully monitor the consistency of the newborn’s stool.
In an uncomplicated pregnancy, the fetus is kept under sterile conditions. But after birth, the child’s body is very quickly colonized by microbes. Therefore, in the middle of the 1st week (usually on the 3rd day), almost all newborns have a transient disorder of the stool.
It becomes more frequent, heterogeneous both in color and consistency. Lumps, mucus may appear in it. Often it is quite liquid, watery. Areas of dark green color may alternate with greenish, yellow and even whitish. Such a chair is also called transitional, and the condition is called physiological dyspepsia. After 2-4 days, these phenomena disappear: mushy stools, homogeneous in consistency, become golden yellow.
Not all children have the same physiological dyspepsia.
Physiological dyspepsia does not require treatment.
Another transitional state observed in newborns is transient dysbacteriosis associated with the formation of the child’s own intestinal microflora. It plays a large role in the digestion of food and the formation of certain vitamins (for example, vitamin K).
During breastfeeding, the intestinal flora of a child is dominated by Bacterium bifidum, a microorganism that has the most beneficial effect on the digestive processes, while artificially — E. coli. With errors in artificial feeding, dysbacteriosis can drag on and cause the child to become ill.
It is quite rare that newborns do not pass meconium. This may be due to intestinal obstruction due to a meconium plug in the rectum, which can only be removed by a doctor, or a severe hereditary disease — cystic fibrosis (cystofibrosis).
In the latter case, the enzymes lipase and trypsin are absent in the digestive juice, as a result of which the meconium becomes viscous and sticks to the intestinal walls. Peristalsis is not able to move it. There is complete intestinal obstruction. As a rule, at the end of the 1st day, the child begins to vomit.
This extremely serious condition of the newborn is called meconium ileus. It is treated only by surgery. There are other causes of obstruction.
Constipation may develop after a successful passage of meconium. However, infrequent bowel movements — for example, every other day — are not necessarily associated with constipation if the child’s stool remains soft.
Most often, this frequency of stools occurs in children who are bottle-fed.
If the stool is delayed for 2-3 days, and then the baby has to push for a long time to empty the intestines, then they say about constipation.
If your newborn has frequent constipation, be sure to bring this to the attention of your doctor.
Chronic constipation in a newborn may be associated with a narrowing (stenosis) of the anus or with megacolon — an expansion of the rectum with a significant thickening of its walls, due to which intestinal motility is weakened. In any case, the child should be under medical supervision.
If constipation is an occasional occurrence, additional fluids usually help the child. If it does not lead to a change in the consistency of the bowel movements, half a teaspoon of sugar is added to the milk mixture. Or after the morning feeding, the baby is given some sweet fruit juice diluted with water (for example, plum).
In rare cases, and better on the advice of a doctor, you can resort to an enema. Often, constipation is a harbinger of a child’s disease (cold or infectious).
If a newborn’s bowel movements become liquid, and before that they looked normal, you should immediately consult a doctor — the baby may have one of the intestinal infections.
At the same time, other signs usually appear: the stool becomes more frequent, its consistency and color change — it becomes greenish or dirty green with white patches, later traces of blood and pus are found in it.
If your baby has mild diarrhoea, continue feeding while you wait for the doctor. Breast milk helps with many types of intestinal disorders. But it is better that the baby eats less.
If a newborn is fed with artificial milk mixtures, then they are half diluted with boiled water. The baby may not eat. Then he is fed little by little, but often.
If the child has severe diarrhea, vomiting occurs, the temperature rises above 38 °C. Dehydration of the body begins, which is very dangerous — the baby looks emaciated, with gray circles under the eyes.
If you cannot get him to the hospital immediately, before the doctor arrives, give your child a drink instead of milk of the following composition: for 250 ml of water — 1 tablespoon of sugar (without top) and a teaspoon of salt.
In some diseases there is also bloody stool (melena) — it is black. This is a sign of heavy bleeding in the upper intestines. At the same time, a red border forms around the stool on the diaper. The child must be urgently delivered to the hospital, he may die.
If the baby is under medical supervision for diarrhea, still be attentive to the child’s condition. It also happens that the prescribed treatment is ineffective, but meanwhile the symptoms of the disease weaken during the water-tea break — the baby definitely feels better. But his health deteriorates immediately after feeding. This is a very important sign, and the doctor should be aware of it. Diarrhea in a child may be due to hereditary intolerance to one
of the sugars of milk or formula. The baby needs diet food.
Diarrhea often occurs with other metabolic diseases.
The appearance of the child’s stool and the consistency depend on what he is fed.



 In this case, you need to contact a pediatric surgeon and undergo an abdominal ultrasound to exclude surgical pathology.
In this case, you need to contact a pediatric surgeon and undergo an abdominal ultrasound to exclude surgical pathology. 
