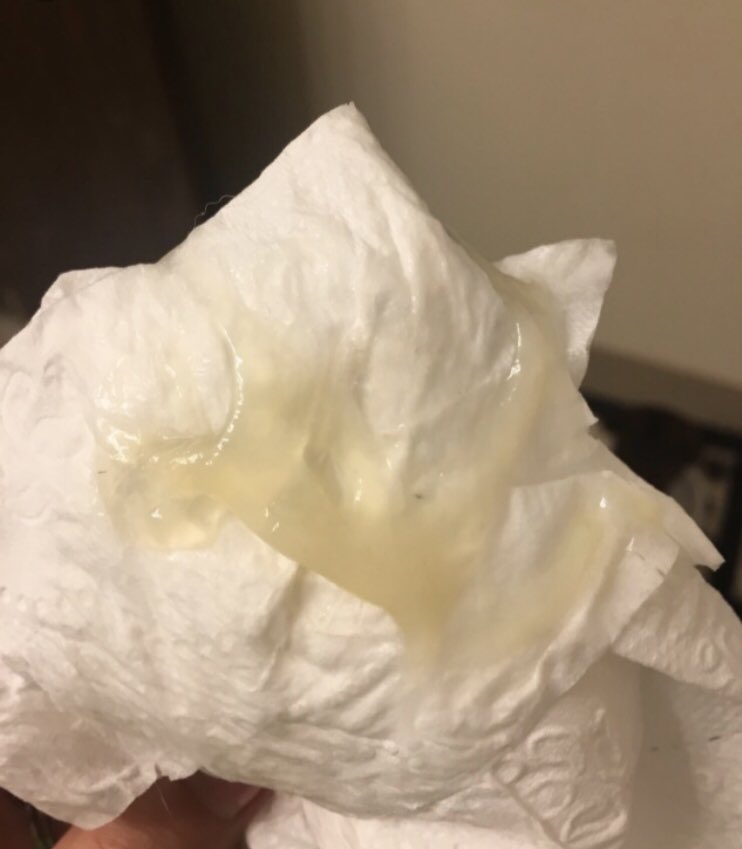
Image of mucus plug: What a mucus plug looks like: photos
Posted onMucus Plug — What Does a Mucus Plug Look Like
Home
/
Pregnancy & Birth
/
Your Third Trimester
/
Losing your mucus plug
Pregnancy by week
1 1
2 2
3 3
4 4
5 5
6 6
7 7
8 8
9 9
10 10
11 11
12 12
13 13
14 14
15 15
16 16
17 17
18 18
19 19
20 20
21 21
22 22
23 23
24 24
25 25
26 26
27 27
28 28
29 29
30 30
31 31
32 32
33 33
3434
35 35
36 36
37 37
38 38
39 39
40 40
Pregnancy & Birth
-
Expand pages
Pregnancy Weeks -
Expand pages
Your First Trimester -
Expand pages
Your Second Trimester -
Expand pages
Your Third Trimester -
Expand pages
Antenatal classes available to you -
Baby Shows -
Pregnancy FAQs -
Expand pages
Pregnancy Health -
Expand pages
Labour -
Expand pages
Preparing for Baby -
Expand pages
Pregnancy yoga classes -
Expand pages
Pregnancy massage near you -
Expand pages
Planning your baby’s nursery -
Expand pages
Your rights and benefits -
Expand pages
Maternity clothing -
Expand pages
Pushchairs & car seats -
Pre-eclampsia signs and treatment -
Expand pages
Pregnancy swimming classes -
Expand pages
Baby loss -
Expand pages
A dad’s guide to pregnancy -
Pregnancy Due Date Calculator -
Early signs and symptoms of pregnancy -
The best pregnancy and baby deals! -
Expand pages
Pregnancy wellbeing -
Expand pages
Postnatal Wellbeing -
Postnatal depression -
The best Amazon Spring Sale deals -
Maternal mental health: A safe space
What is a Mucus Plug?
Early in pregnancy, mucus from the cervix thickens to form a plug. This mucus plug seals the entrance to the womb to protect the developing fetus. As well as being a physical barrier to bacteria and other things that could harm the fetus, the mucus plug
also works with the body’s immune system to kill viruses and bacteria.
What does the mucus plug look like?
When the mucus plug is discharged from the vagina it is known as a ‘show’. This usually happens when your pregnancy has reached term (after 37 weeks), and is a sign that the cervix is softening ready for birth.
The plug may come away whole or in several pieces, and it is normal to lose a small amount of blood mixed with the mucus.The show is a small amount of sticky, jelly-like, snot, brown mucus that
can be clear, but is more often pink because of the blood that is lost at the same time. It can sometimes be difficult to tell the difference between the mucus plug and the normal vaginal discharge that occurs during pregnancy.
Here are
a couple of photos from our mums:
When does the mucus plug fall out?
This usually happens when your pregnancy has reached term (after 37 weeks pregnant).
Does your mucus plug come out before or after your waters break
Your mucus plug is likely to come away before your waters break, although some women never notice losing their mucus plug.
Does losing the mucus plug mean you are about to go into labour?
While the show usually happens shortly before or after the start of labour, labour
may not start for a few days, and in some cases, a couple of weeks after a show, however, please remember that not every woman will have a “show”.
What happens if I lose my mucus plug in early pregnancy?
If you lose your mucus plug before 37 weeks, you should inform your midwife or hospital immediately. Early loss of the plug may be a sign of early (premature) labour, other signs of labour such as increased fluid leaking from the vagina (waters breaking) or period-like pains in your abdomen or lower back. However, losing your mucus plug early does not mean that you will go into labour immediately, and it could be a couple of weeks before labour begins.
When should I call the doctor/hospital?
If you continue to lose blood after the show, it may mean that something is wrong and you should contact your midwife or hospital immediately.ou should also contact them if the plug is green or has a foul smell, as these may be signs of infection.
Mum’s experiences of losing their mucus plug
Here, at Emma’s Diary we’ve asked our mum’s what happened when they lost their mucus plug, here’s what they had to say…
I lost a tiny bit at 39 weeks but didn’t really notice it. Lost mine in labour after my waters broke at the hospital, had to ask for tissue as I was walking/moving about through labour so it was coming out as my waters were trickling out too 😂Natalie
I lost mine just before my waters broke. I ran up to the toilet and as I got there my waters went. I think I had been loosing bits a few days before but nothing massively noticeable. I was 37+5 when my waters went and I had my baby girl later
that day.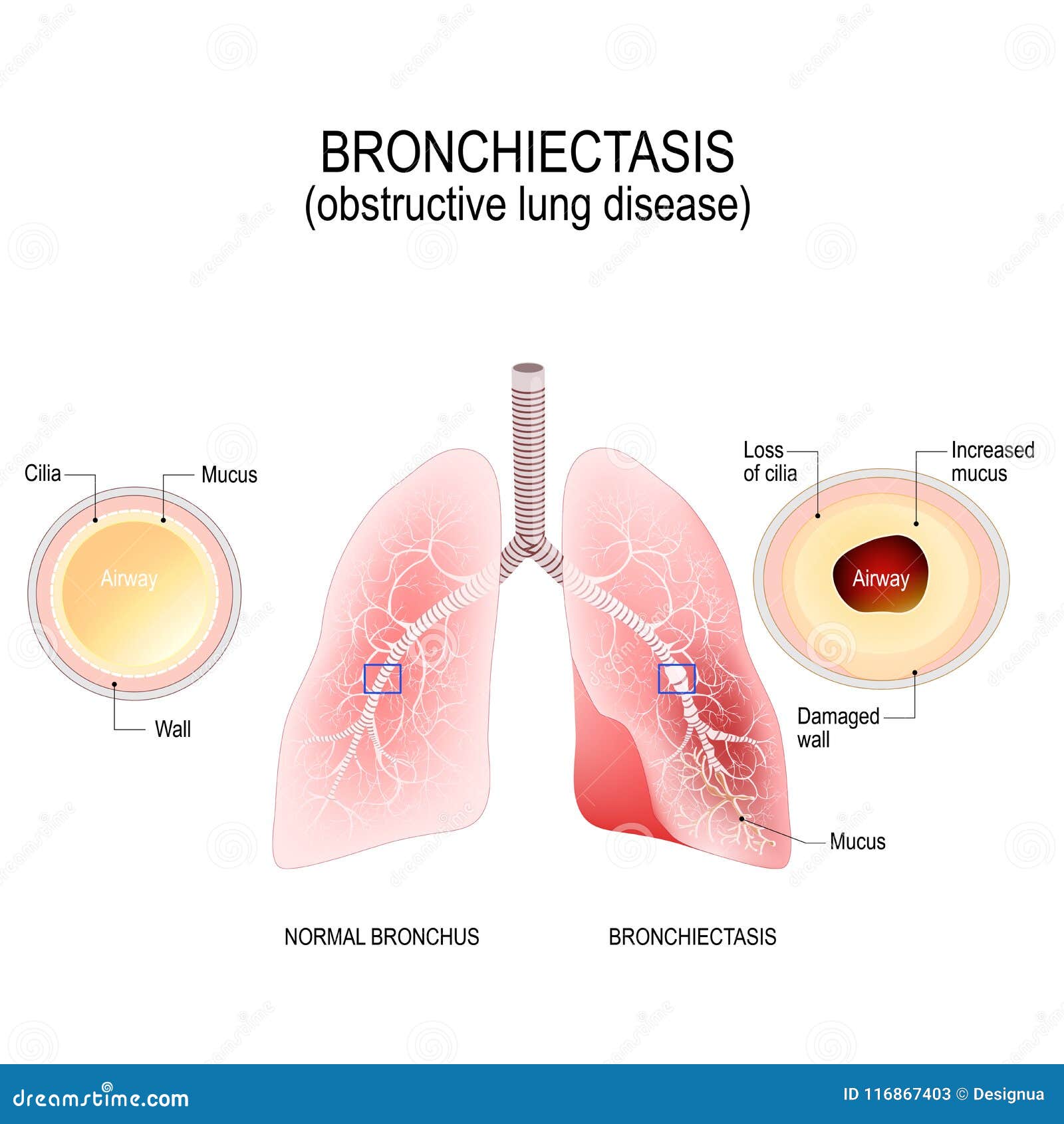
Ruby
I lost my mucuos plug at 38 weeks with my eldest, I remember coming out of the bathroom terrified that this was really happening, my partner asked why I looked so pale think as a first time parent it can be quite scary I thought I’d go into
labour quickly after that from what I’d read, but it made no difference my daughter arrived safely an hour before her due date.
Sinead
I lost mine over a number of weeks! I think it was about 3 weeks or so before I gave birth. I thought things were happening but obviously not . It was like a mixture of end of period kind of discharge with mucuous etc. I wasn’t expecting
it to go on and on for weeks I didn’t read anything that said that.
Amy
This content is sponsored by Pampers®
THE LATEST HOT TOPICS
The importance of Vitamin D
Get all the facts here.
Read more
10 items every new mum loves
Here’s a list of must-have items to get you through those first few weeks after birth…
Read more
Why you’ll LOVE a pregnancy pillow
Here’s how it can help you during your pregnancy…
Read more
JUST FOR YOU
Your hospital bag checklist
Make sure you have everything you need
Read more
Find the perfect car seat & pushchair
Here are a few things to keep in mind…
Read more
Everything you need to know about giving birth
We answer your most common questions…
Read more
Emma’s Quick Links
Is it The Mucus Plug Or Discharge?
In early pregnancy, your body creates a barrier between the outside world and your developing baby.
The cervical mucus plug is something you don’t really think much about – at least, not until you get to the end of pregnancy and you start to look for the signs of labor.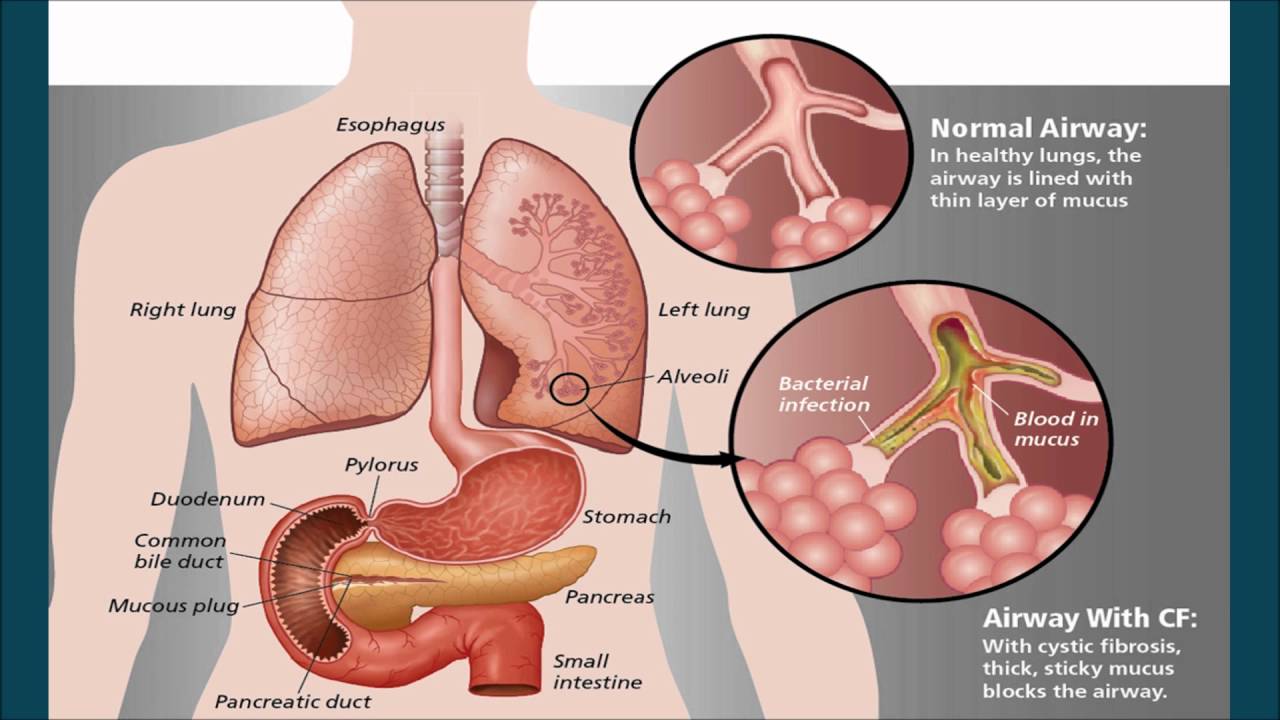
Does seeing the mucus plug necessarily mean labor is imminent, is it the plug or discharge?
Let’s find out everything about the mucus plug.
What is a mucus plug?
Your baby is inside the amniotic sac inside your uterus.
The cervix is a canal of tissue that joins the vagina and the uterus. At the early pregnancy stage, a thick jelly-like fluid mucus plug forms in your cervix to protect your baby from infection.
The plug is a collection of mucus that accumulates in the cervical canal.
The mucus has antibodies to protect your baby from bacteria, viruses and infections. It provides vital protection for you and for your baby’s health.
You might be surprised at how much mucus is collected in your cervix. That’s because the cervix continues to make the mucus and amazingly regenerates.
When do you lose your mucus plug?
As your body prepares for birth, the cervix starts to thin. Thinning (or effacement) allows the cervix to dilate during labor.
As the cervix thins, it will also dilate a small amount, allowing the mucus plug to loosen and come away.
This process can happen over several weeks before you actually go into labor. Some mothers, especially those having their second baby, won’t notice any signs their cervix is thinning until they’re actually in early labor.
Mucus plug or discharge?
Many women find they have a lot more vaginal discharge during pregnancy. This can be clear, white or creamy; it is odorless.
Check out Discharge During Pregnancy | What’s Normal and What’s Not for more information.
It can be difficult to tell whether what you’re looking at is just more discharge or your mucus plug.
The mucus plug is usually a jelly-like, thick, snotty, stringy or even sticky discharge.
It can be tinged with pink, red or even brown. This happens when small blood vessels break as the cervix starts to soften and thin.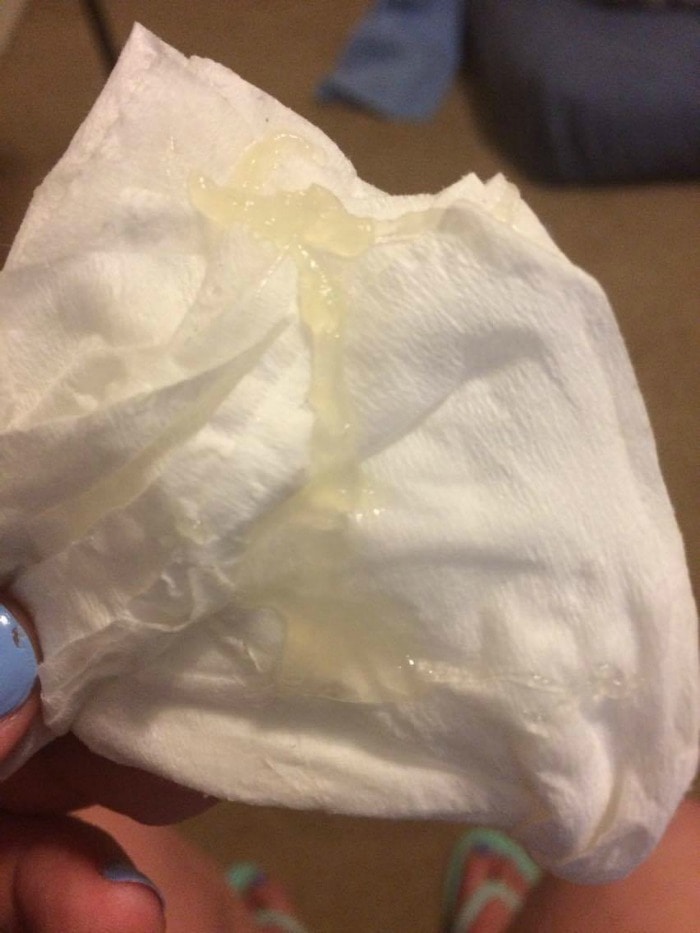
In pregnancy, you can have many different types of vaginal loss and it can be difficult to tell what it is. You can send a pic to your healthcare provider, or describe what it looks like.
Find out more in our article What Does A Mucus Plug Look Like? Losing The Mucus Plug.
Can mucus plug come out slowly?
Some women don’t even notice their mucus plug because it comes out slowly over a few days, or even weeks.
You might see it as one obvious blob of mucus plug, when wiping with toilet paper, or you might notice an increased vaginal discharge over a few days. If you lose the mucus plug all at once, it might have an obvious plug shape, about 4-5cm long.
If you’re not sure what your vaginal loss actually is, pop a sanitary pad on it and keep an eye on the amount and color of the discharge.
You can show the pad to your doctor or midwife if you’re unsure or have concerns.
Don’t worry; they have seen all kinds of bodily fluids before and won’t mind what it looks like.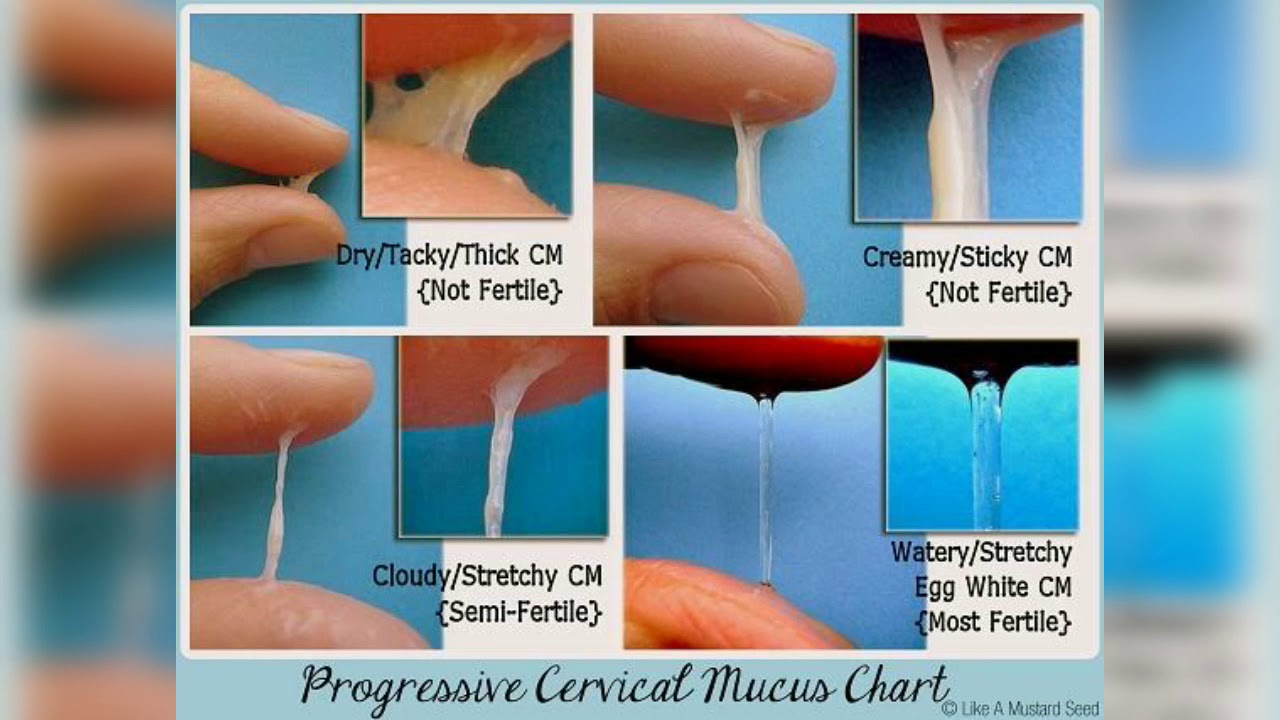
What does losing your mucus plug mean?
Losing your mucus plug might be one of the early labor symptoms. It means labor is approaching as the cervix begins to open up and the thick plug is released.
As mentioned earlier, your cervix is starting to ripen and thin. This is the pre-stage of labor.
Labor might still be some days away, but it’s OK to get a bit excited. More about this later.
If you start to lose your mucus plug, it’s a good signal to you and your birth partner to slow down and take good care of yourselves.
Make sure you have lots of sleep and good food. You will need the energy later, when labor starts.
Maybe you could put the last few things in your labor bag, then relax as best you can. Your baby is coming soon and you’ll need all the rest you can get before labor begins.
Mucus plug color chart
The mucus plug discharge can have different colors and most of them are okay. Let’s see the reasons for the different colors.
1. White mucus plug
Most parts of the mucus plug are whitish in color. The mucus plug is a lot of mucus together and it takes on a creamy color (you can see I’m avoiding saying ‘white’).
2. Brown mucus plug
As the mucus plug forms over many weeks, any small blood vessels that break in the cervical canal would tinge the mucus plug. The blood would become part of the plug and turn brown.
3. Pink mucus plug
If there is a pink color in your mucus plug, this comes from freshly broken little blood vessels around the cervix. There isn’t a lot of blood and it mixes well with all the mucus, so the plug has a slightly pink tinge.
4. Green mucus plug
Green has never been a good color for stuff coming out of your body, right?
However, we’re talking about mucus and a plug made of it.
Research shows that the cervical mucus plug inhibits ascending bacteria but it doesn’t completely block it.
In that case, how do we differentiate simple mucus from a possible infection?
Although common sense goes a long way here, I’d suggest calling your healthcare provider.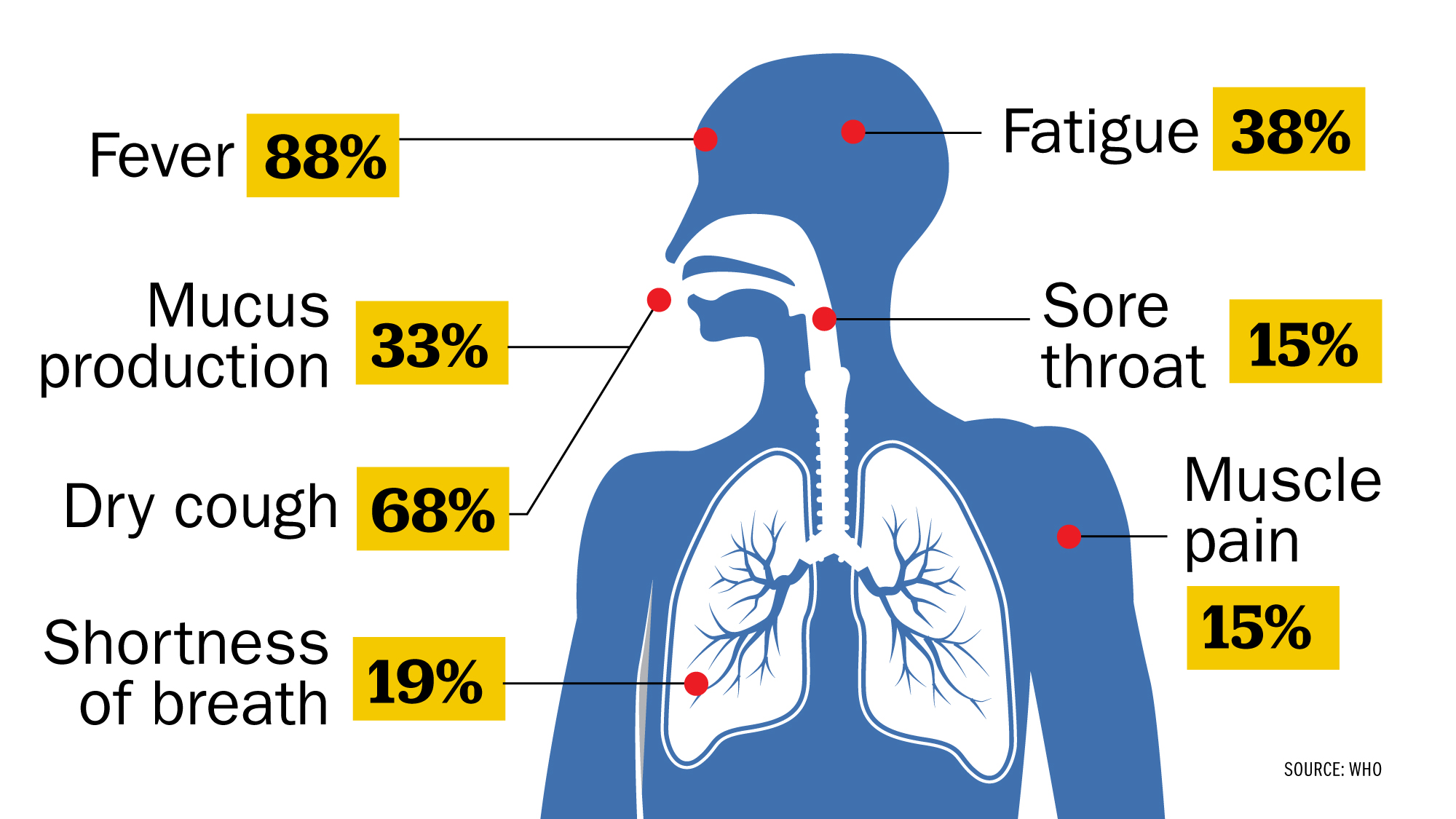
5. Red mucus plug
Sometimes the mucus plug comes out when there’s more cervical activity and several small blood vessels break and make the plug blood-tinged.
Bright red blood is always scary. If the blood mixes well with the mucus and you don’t see clots forming, it’s an okay amount of bright red blood. Here the red mucus plug is accompanied by a bloody show.
If you see blood clots, though, call the emergency services, as this is considered heavy bleeding.
Do I need to call my healthcare provider?
Losing your mucus plug is exciting but it might be a while before labor starts. It’s best just to rest and be prepared.
You should call your doctor or midwife, however, if:
- You see a lot of bright red bleeding. This could be a bloody show or it could be a sign of problems with your placenta
- The mucus plug is green.
As discussed, any green vaginal discharge is a ‘NO’
- You notice a foul odor. This could be a sign of infection (the color might also be green)
- You’re under 37 weeks of pregnancy. This might be a sign of preterm labor
- If your water breaks or you are unsure or worried about the color. Water breaking isn’t always a sudden gush of clear fluid.
- You have persistent pain. Pain is never normal. If you experience pain, even if you have your typical vaginal discharge, contact your provider.
Remember, losing your mucus plug is one of many other labor symptoms. You can put a sanitary pad on if you’re not sure about any vaginal leaking or bloody show. Keep your pad or panty liner, in case you need to show the doctor. If you’re concerned about anything, call your healthcare provider for advice.
How long after losing the mucus plug does labor start?
To lose your mucus plug is only one of a number of signs that labor is beginning.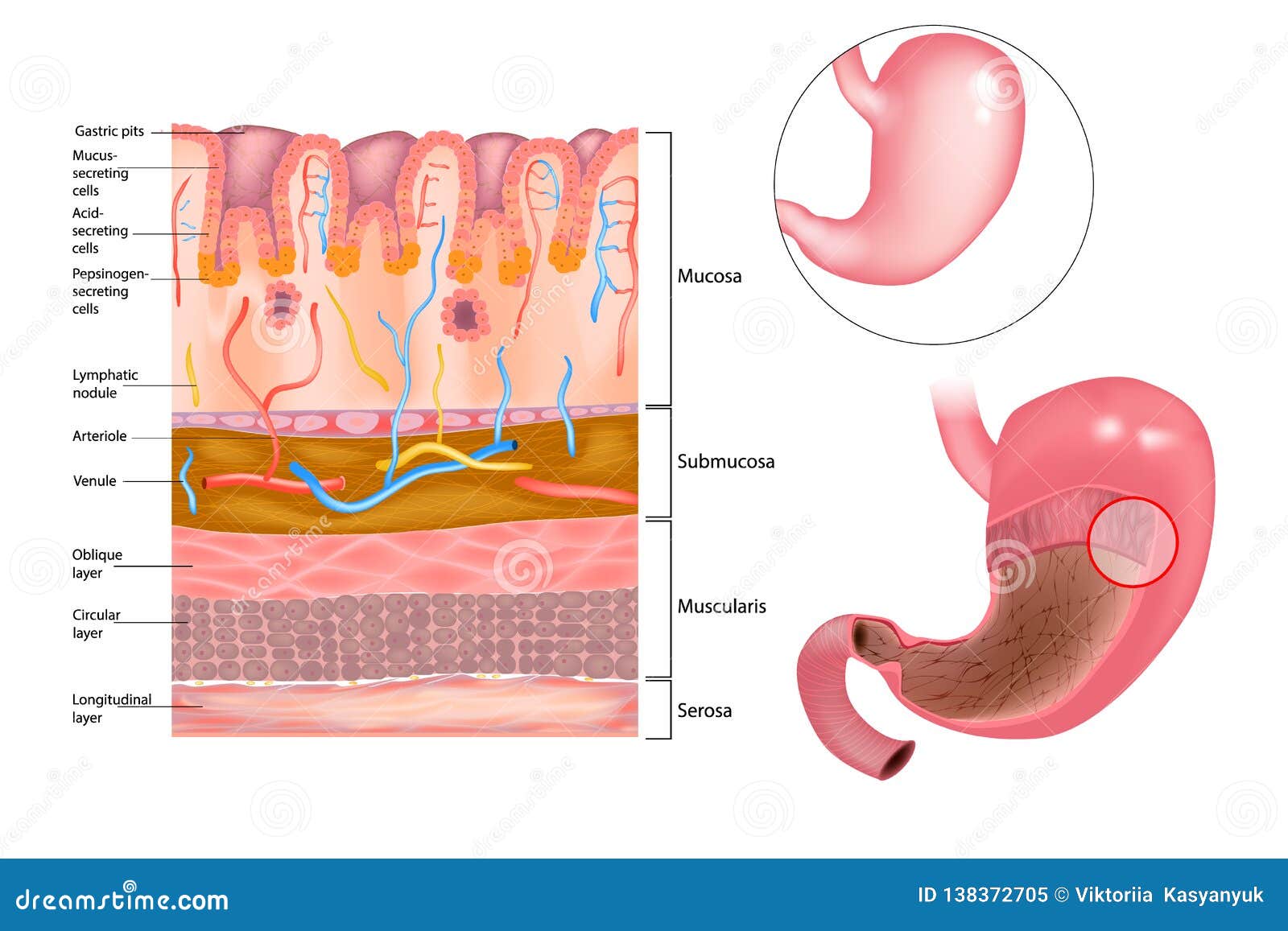
Look at our article Signs Of Labour | Could I Be In Early Labour? for other signs you might notice.
Every woman is different, and every pregnancy and every labor is different.
A member poll in the BellyBelly forums showed:
- 45% of women lost their mucus plug 1-2 weeks before labor started
- 34% saw their mucus plug 2 days before labor began
- 30% of women lost their mucus plug during labor
- Around 17.65% didn’t see theirs at all.
Can you lose your mucus plug more than once?
If the mucus plug comes out gradually, it might seem like it’s happening more than once; in fact, it’s just more of the same.
The cervix regularly makes more mucus during pregnancy so there can be a lot of mucus to lose. Even when you think you’ve seen the entire mucus plug, you might still see some more later.
Interestingly, many women will have another mucus bloody show just before they are ready to push their baby out.
The bloody show happens when the cervix is fully dilated and the baby is moving down the birth canal.
What should I do if I lose my mucus plug?
Losing the mucus plug is a sign of the cervix softening and that’s brilliant. Your cervix prepares as labor approaches.
If you lose your mucus plug at 37 or more weeks pregnant and it looks normal, even if you feel a bit of pelvic pressure, then you don’t necessarily need to do anything.
You might want to call your doctor or midwife, especially if you’re anxious about birth or if you go into labor soon after.
But there’s no need to do anything if you lose your mucus plug. Labor contractions could be some time away so it’s great just to carry on with normal life and see what happens.
You can practise your breathing and relaxation techniques, in preparation for when early labor contractions start.
Unless friends and family are part of your support team, you don’t need to let them know things are happening just yet, or they might want progress updates.
This can make you feel you’re under pressure, like a watched pot! It can stall any contractions you were having and slow things right down.
It’s best to tell just your birth partner. This time is all about you and your baby.
Get plenty of rest, eat well and stay hydrated. Finish packing your labor bag and chill.
Good things are happening and labor is not too far away.
9 ineffective methods of treatment in otolaryngology. Evidence-based medicine perspective
Over the past 10 years, otolaryngologists have received a lot of new data about diseases and methods of treatment. For example, it was previously believed that the removal of adenoids reduces immunity. And in 2019, scientists found out that this is not the case.
However, the MOH clinical guidelines—instructions for physicians to make a diagnosis and prescribe treatment—do not change as quickly as new high-quality studies come out. Unfortunately, because of this, many doctors continue to prescribe treatment, the effectiveness of which was refuted several years ago.
In this article, we have collected 9 outdated methods and told what evidence-based medicine uses in otorhinolaryngology.
There is no evidence that a course of tonsil flushing reduces the incidence of «plugs»
Tonsil washing
This is a fashionable but almost always unnecessary procedure.
Let’s explain why.
The tonsils are sponge-like in structure and can absorb food debris and dead bacterial cells. Their accumulation is called «plugs» or tonsillolites.
This is what the «plugs» in the tonsils look like
Previously, otolaryngologists believed that “plugs” were one of the manifestations of chronic tonsillitis. And tonsillitis, in turn, is dangerous for the heart, kidneys and joints. Therefore, doctors prescribed five to ten washing procedures. And along with this, testing for rheumatoid factor and C-reactive protein, which show the detrimental effect of tonsillolitis on the body.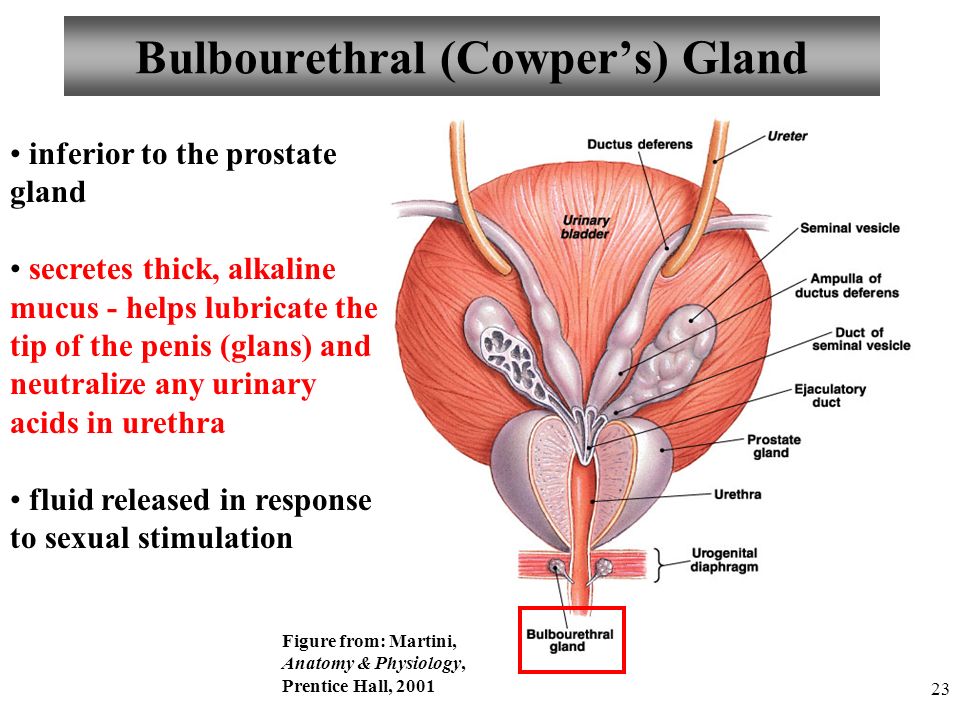
However, the connection between «plugs» and tonsillitis has not been proven. Tonsillitis is a bacterial disease that in 80% of cases is caused by beta-hemolytic streptococcus, in the rest — other bacteria and fungal microorganisms.
By themselves, «plugs» are not a disease and do not require treatment. When there are too many of them and this causes discomfort, you can wash the tonsils, but only once or twice. This should be enough. If discomfort or bad breath persists after the procedure, the otolaryngologist should investigate the cause.
Most often, gastroesophageal reflux is to blame: the reflux of stomach contents into the larynx enhances the appearance of “plugs”.
Sometimes «plugs» occur for no reason: this happens in 3% of patients. They have to periodically wash or remove the tonsils.
Prescribing antibiotics for safety net
Another technique that has not proven its effectiveness is local antiseptics for tonsillitis.
The standards also require doctors to prescribe antibiotics. But the essence of evidence-based medicine is not to prescribe unnecessary drugs that can harm. First, the doctor must assess the likelihood of streptococcal infection using the Zentor and McIsaac scale.
The scale shows the likelihood of group A beta-hemolytic streptococcus
Depending on the number of points, the doctor prescribes a streptatest and culture for group A beta-hemolytic streptococcus. A positive result indicates an episode of acute tonsillitis. In this case, the patient needs a ten-day course of antibiotics.
If in the last year you have had seven such episodes, or five in two years, or three in three years, the tonsils require removal. But the usual sore throat does not count: only confirmed streptococcus.
Nasal lavage with Cuckoo apparatus
The Proetz Nasal Wash, also known as the Cuckoo Nasal Wash, is a procedure used for inflammatory conditions such as sinusitis. It helps the outflow of fluid accumulated in the sinuses during edema.
The procedure looks like this: a saline solution is injected into one nostril, sometimes furatsilin or dioxidin. A vacuum suction is inserted into the other nostril, which draws fluid from the nose. The patient during the procedure must make the sound «cuckoo» so that the liquid does not get into the throat.
Flushing with saline at home is no less effective than the «cuckoo» and painless
Modern evidence-based medicine does not recognize this procedure. First, side effects are possible — nosebleeds or even more swelling. Secondly, home rinsing of the nose can be no less effective and comfortable: “cuckoo” is a painful procedure.
In world medicine, Proetz lavage is not used at all, only home lavages are used there using devices such as the Dolphin.
Small incision in the eardrum to drain pus
Eardrum puncture
The method of the Soviet school to combat purulent otitis media is a puncture of the eardrum. The logic was this: when pus accumulates in the middle ear cavity, it provokes pressure on the eardrums and can spread to neighboring tissues. Therefore, doctors artificially made an incision, gently releasing pus.
Modern otorhinolaryngology follows a different tactic: the patient takes a long course of antibiotics with high doses. After it, as a rule, purulent otitis media disappears.
But in some cases, antibiotics do not help, and then you have to turn to a puncture of the eardrum. For example, in our practice there was a case when a course of antibiotics did not help a two-month-old baby. He had a relapse, and pus got into the behind-the-ear area.
Maxillary sinus puncture
In the past, puncture was often used to clarify the diagnosis of sinusitis. Moreover, the indication for this procedure was the blackout on the x-ray. It can mean accumulation of fluid. A special curved needle was inserted into the patient’s nose, with which pus was removed from the sinus, then it was washed with an antiseptic. The fluid obtained during the puncture was sent for examination. However, in the vast majority of cases, this procedure is not necessary, and many patients can be treated conservatively.
There is no evidence for the effectiveness of the Minin reflector (blue lamp). But we know about the dangers of blue light for the retina, especially in children.

Blue lamp, electrophoresis and other «magic» physiotherapy
To begin with, let’s define the terminology: in Russian and Western medicine, physiotherapy means different procedures. In English-speaking countries, this is exercise therapy for recovery from surgery, injury and past illnesses.
In Russia, physiotherapy is understood as the effect of microcurrents, magnets and mud therapy. Physiotherapy in otorhinolaryngology is a common direction. But if earlier patients were offered to “disinfect” the nasal mucosa with the help of a blue Minin lamp, then electrophoresis with Lidaza is still used for exudative otitis media. This is a procedure in which a cotton swab moistened with the Lidaza enzyme preparation is inserted into the ear canal. With the help of microcurrents, the drug must penetrate inside and dilute the liquid.
However, there is no evidence of the effectiveness of this method. The same as with treatment with mud, magnets and salt in caves.
I’ll give you an example. With laryngitis — inflammation of the larynx — inhalation is often prescribed. The patient is offered to breathe mineral water or saline. But it has been proven that inhalations do not cure laryngitis in either adults or children. But they add excess fluid to the bronchi and alveoli. Because of this, it is more difficult for the patient to expectorate and it is difficult to breathe.
Another frequently prescribed procedure is laryngeal infusions: the injection of hormones into the vocal cords. The method promises a quick restoration of the voice. But this method is dangerous: injection can provoke a spasm, which sometimes ends in asphyxia (suffocation).
Instead of these dangerous and complex approaches to the treatment of laryngitis, evidence-based medicine methods are used: maintaining voice rest, drinking plenty of water and humidifying the air in the room. If you urgently need to get rid of hoarseness — start a course of corticosteroids.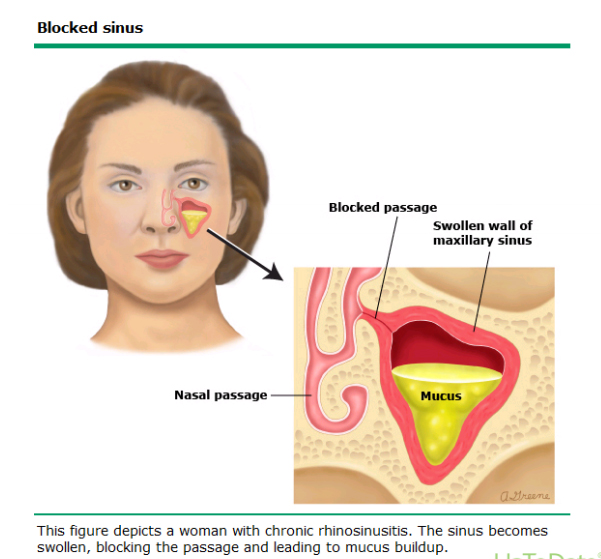
X-ray of paranasal sinuses
Previously, with any suspicion of sinusitis, the patient underwent an x-ray of the paranasal sinuses. This is not the most reliable method: not all angles are visible in the pictures, and any darkening was interpreted in favor of sinusitis. But the darkening of the sinuses indicates the reaction of the mucosa to a runny nose.
Whereas the diagnosis of «sinusitis» can be made as a result of examination and questioning of the patient. About sinusitis is evidenced by the duration of the disease, the presence of high fever, pain in the head and a number of other signs. If the otolaryngologist doubts the diagnosis, for example, when the nose is healthy on examination, but the sinuses hurt, he will prescribe not an X-ray, but a CT scan. This is a more informative method that allows you to see the most important thing — the sphenoid sinus. This is necessary to exclude deadly thrombosis of the cavernous sinus.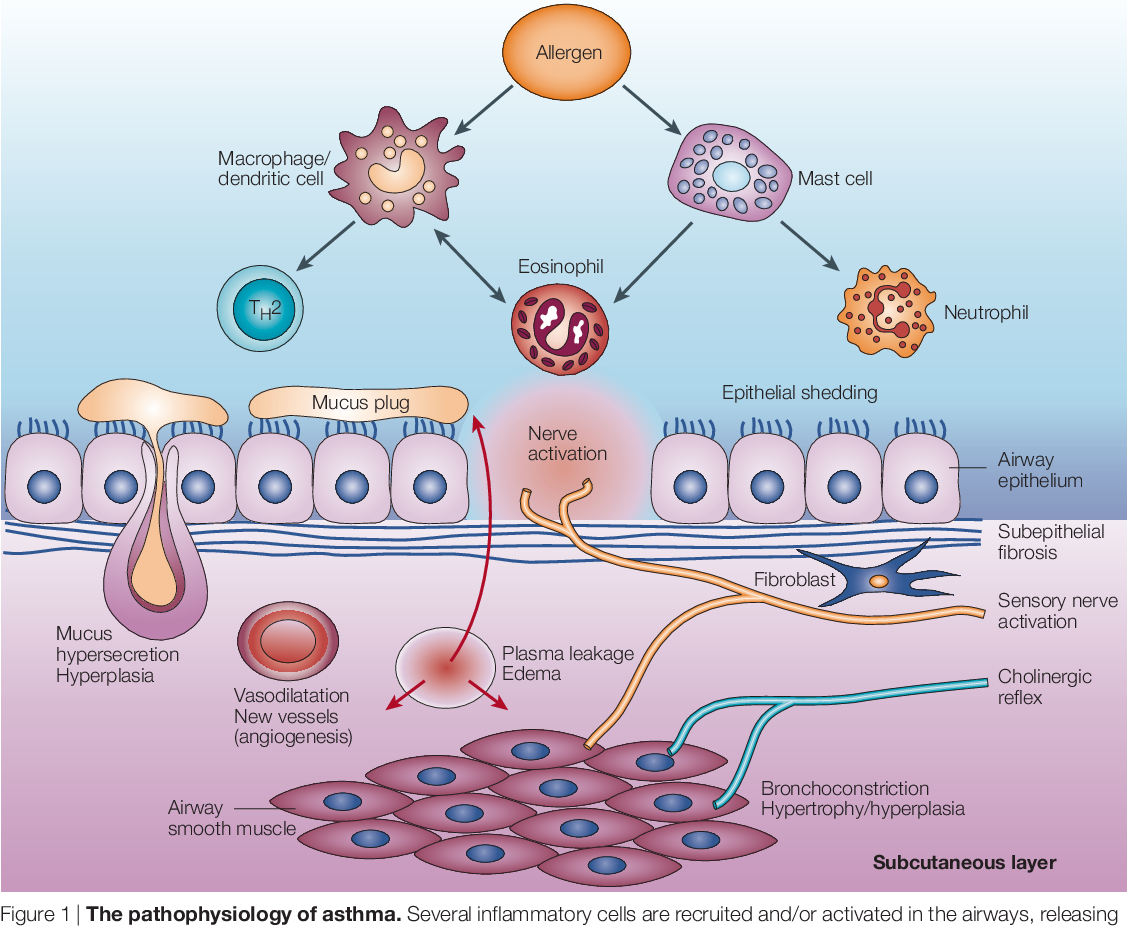
Beckman’s adenotom
Blind adenoid removal
The pharyngeal tonsils perform a protective function: they prevent the entry of pathogenic microorganisms into the body. But sometimes, due to a strong immune response to infections, the tonsils grow. In this state, they are called adenoids. They can grow and close the entrance to the auditory tube, after which the child will lose his hearing. Therefore, in ENT practice, a procedure for removing adenoids is common.
Previously, it was carried out like this: the child sat in a chair so that he would not twitch, tied his legs and arms and held his head. The surgeon inserted Beckman’s adenotome, an instrument with a metal ring at the end, which was invented over 100 years ago, into the nasal passage. And then pulled out the adenoids. This tool and technique was used until the 2010s.
Then, to remove the adenoids, they began to use a shaver — a thin tube with a cutter at the end.
Thanks to endoscopes, doctors saw the unsightly consequences of blindly removing adenoids. For example, rough scars on injured pipe rolls. Because of them, the patient is more likely to get acute or exudative otitis media. In addition, endoscopes have increased diagnostic capabilities in medicine.
The doctor inserts an endoscope to diagnose ENT diseases
Hormone injections
Previously, doctors believed that injections were more targeted at fighting the disease. Therefore, intranasal blockades were popular — injections with hormonal drugs such as dexamethasone or hydrocortisone. They helped reduce the volume of mucous in the nasal cavity.
Now doctors prefer sprays: mometasone, fluticasone or budesonide. They proved to be much more effective than injections. Hormones, if they are injected inside, are absorbed too intensively: up to 80% of the drug is absorbed into the blood and systemically affects the body. And preparations in the form of sprays are absorbed by less than 1%.
***
Many of the procedures described here seem inhumane and out of date. But, fortunately, over the past 10 years, medicine has stepped forward and many of the old methods have ceased to be applied. In our clinic, we follow the principles of evidence-based, and therefore modern and humane medicine.
Sources:
- Pavlov V.V., Lopatin D.G. Optimization of methods of surgical treatment of chronic laryngitis, precancerous diseases of the larynx // Acta Biomedica Scientifica, 2014
- Asilbekova Zh. A. Modern methods of treatment of fungal diseases of ENT organs // Bulletin of Surgery of Kazakhstan, 2012
- Zarubin M.
M. Treatment of diseases of the ENT organs. The latest reference book // Phoenix, 2007.
- Palchun V. T. Otorhinolaryngology // GEOTAR-Media, 2008.
Treatment of inflammatory diseases of the paranasal sinuses in Odessa
- Diseases of the NOSE
- Inflammatory diseases of the paranasal sinuses
The paranasal sinuses are cavities in the bones of the skull that are connected to the nasal cavity through small openings (ostia). The biological role of these voids is to reduce the mass of the skull, in addition, they are resonators and give the voice of each person its own unique timbre.
Polyps do not just happen. This is the reaction of the mucous membrane to chronic irritation. The process of polyp formation can be figuratively compared with the appearance of a blister and callus on the foot when wearing uncomfortable shoes.
There are several paranasal sinuses:
- Grids (ethmoid labyrinth) — many small cavities in the thickness of the ethmoid bone.
- Maxillary sinuses (maxillary sinuses) — named after the medical scientist who first described it).
- Sphenoid sinus.
Sinuses are not closed cavities!
Figuratively, the sinus can be represented as a bottle with a narrow neck, and this neck «opens» into the lumen of the nasal cavity. The necks, and according to the scientific fistula of all sinuses, except for the sphenoid, open in one specific place — under the middle nasal concha.
See how it looks on the diagram using the maxillary and frontal sinuses as an example.
The maxillary sinuses (D) have an outlet fistula from above, and the frontal sinuses (L) have a bottom, as if bottles turned upside down.
This scheme is, of course, exaggerated. In life, everything is somewhat more complicated…
Why is this necessary?
Each sinus is lined on the inside with a mucous membrane, the same as the nasal cavity. The mucous membrane, despite its apparent tenderness and vulnerability, is a powerful protective barrier, impenetrable to most infections.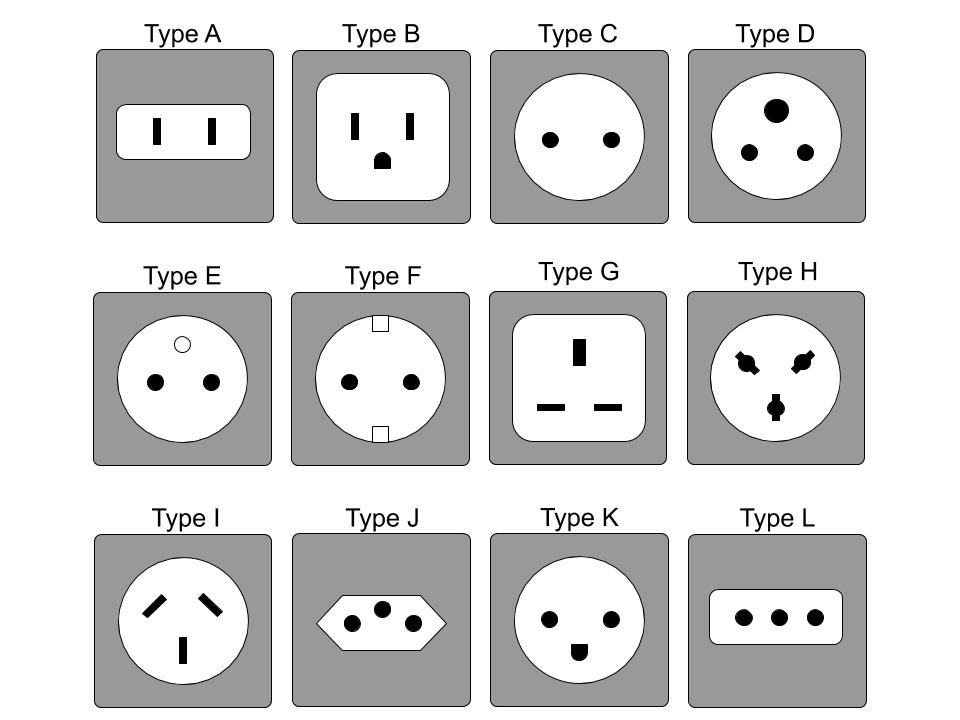
The mucous membrane produces mucus, which contains a number of protective substances that neutralize microbes. The process of mucus formation is constant, so it must be constantly removed. For this, fistulas are needed — through them, mucus is discharged into the nasal cavity.
Fig. 3 Computed tomography of the paranasal sinuses. The arrows point to the excretory fistulas of the maxillary sinuses.
Moreover, it is not diverted by «gravity». The surface of the mucous membrane is covered with microscopic cilia. These cilia are in constant motion and it is they who move the mucus towards the sinus fistula.
When a person becomes ill with a respiratory viral infection, the secretion of mucus in the nose and sinuses increases. If the fistula of the sinus has a sufficient diameter (for large sinuses it is 2.
If the size of the anastomosis is less than necessary, the mucus cannot come out and the sinus begins to fill with it. There is a feeling of pressure and fullness in the projection of the sinus.
There are 3 reasons why the sinus fistula can be narrowed:
- Severe swelling of the mucous membrane surrounding the anastomosis (typical for some respiratory viral infections).
- Individual anatomical features (naturally narrow fistula).
- Volumetric pathological process in the fistula zone: polyp or tumor, hypertrophy of the middle shell, curvature of the nasal septum in the upper section.
Although nasal mucus is a cocktail of antimicrobial substances, when the mucus stagnates, their activity decreases and it turns into a nutrient «broth» for microorganisms, which the latter certainly use. When a microbial infection attaches, the mucus turns into pus — it becomes cloudy, acquires an unpleasant odor.
This is how the main symptoms of inflammation in the sinus are obtained — pain in the projection of the sinus, purulent discharge from the nose, intoxication (fever, weakness)
Both one and several sinuses can become inflamed. Inflammation of the maxillary sinus is called sinusitis, frontal sinus — frontal sinusitis, ethmoid labyrinth — ethmoiditis, sphenoid sinus — sphenoiditis.
DIAGNOSIS:
The main problem that needs to be solved when examining patients with sinusitis is because of what the fistula blockage occurred. Which of the three reasons (see above) narrowing of the sinus fistula is present in this particular patient. The treatment algorithm and prognosis depend on this.
If inflammation in the sinus is caused by cause No. 1 (swelling of the mucous membrane surrounding the anastomosis), then in the vast majority of cases, a victorious result can be achieved with medication, without punctures and other invasive manipulations. If the reasons are #2 and #3, be sure that without surgical expansion of the anastomosis it is impossible to achieve normal sinus drainage and, accordingly, a long-term result.
The first step is a diagnostic nasal endoscopy. Endoscopy allows, under a 30-fold magnification, to examine all the structures of the nasal cavity, to approach the exit point of the anastomoses and see if there is discharge from the sinuses and if there is something in the nasal cavity that impedes the outflow from under the middle shell.
Computed tomography of the paranasal sinuses is performed in order to see what is happening inside the sinus itself and to trace the entire excretory path from the sinus. This is an x-ray. However, unlike a traditional X-ray, a CT scanner allows you to perform a three-dimensional scan of the body area under study and obtain images with the highest resolution. Images obtained with a tomograph have an incomparable diagnostic value.
This is how the normal middle turbinate area should look like.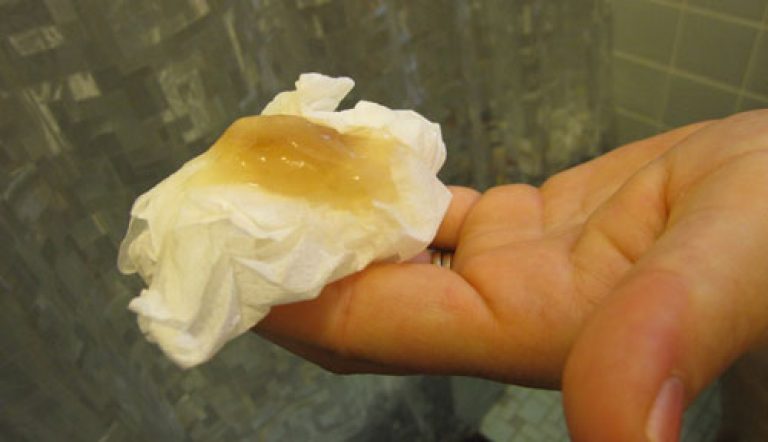
The gap between the middle sink and the partition must also be 3 mm. It’s called the olfactory cleft because it’s where the odor receptors are located.
Anatomy of the middle shell is normal. A cloudy discharge is released from the anastomosis of the sinus. Outflow is free. With such sinusitis, you can deal with medication.
Sinus puncture and drainage, as well as other invasive measures, are not indicated!
Hypertrophied (enlarged) middle shell. It has such large dimensions that it fills the entire space between the partition and the side wall.
Such a sink as a cork closes the outflow from the anastomosis of the maxillary sinus. The patient has chronic purulent sinusitis.
Surgical treatment is required — partial resection of the middle shell. This will restore the outflow from the sinus and permanently save the patient from exacerbations of sinusitis.
A tiny polyp has just emerged from under the middle shell. It also closes the fistula of the sinus and provokes chronic sinusitis in this patient on the right. Such a polyp can only be seen with an endoscope!
In order to save a person from sinusitis, surgical treatment is necessary — removal of the polyp.
Similar situation, larger polyp.
Pay attention to the photo. This patient has no problems on the right half of the nose, but on the left there is a thickening of the septum in the upper section. This thickening (red arrow) presses the normal shell (*) against the side wall. It turns out that it closes the outflow from the anastomosis. As a result — chronic sinusitis and frontal sinusitis on the left.
TREATMENT:
Background.
It is surprising, but at the end of the 19th century, the German professor A. Onodi investigated and described in detail the anatomy of all paranasal sinuses and their excretory fistulas.
All acute inflammatory processes in the sinuses were treated with Proets lavage (known to many under the name «cuckoo») or sinus punctures with washing out of pus and the introduction of antiseptics. But that was the 19th century! Antibiotics have not yet been invented, so the doctors tried their best to alleviate the suffering of the patient. In the 50s of the 20th century, it became clear that we (doctors) were doing something wrong. New knowledge about the structure and functioning of the sinuses appeared and accumulated.
Unfortunately, domestic medicine turned out to be the hardest to climb! Only in 1991, a group of professors from the CIS in the amount of 10 people was invited to Austria in the city of Graz to teach the basics of endoscopy. Among them was my respected teacher, Professor Serafim Zakharovich Piskunov.
It is very sad, but to this day in most medical institutions punctures and cuckoos are widely used, radical operations are carried out. These procedures are unpleasant for the patient, and most importantly, they do not always cure sinusitis!
If there is any anatomical disorder in the nasal cavity that impedes the natural outflow of contents from the sinus, it is necessary to perform a low-traumatic endoscopic operation to eliminate it.
Endoscopy after surgery. Under the control of optics, several cells of the ethmoid bone under the middle shell were removed, which made it possible to open the fistulas of the inflamed maxillary sinus (large arrow) and other lattices (small arrows). New fistulas are wide, pus is not released from them, the patient is cured.
If there is no anatomical fistula block, but the patient has a pronounced pain syndrome and it is necessary to remove pus from the sinus, we use the YAMIK catheter. It is an effective and painless alternative to the traditional piercing.
*** Use of site materials only with the permission of the author and a link to the source.
How to find us
Consultative reception and operations of the otolaryngologist Zaporozhchenko Pavel Aleksandrovich are carried out at the Artmedium clinic.
Clinic «Artmedium» is located at Odessa, st. Nedelina, 78
Appointment for a consultation from Monday to Saturday,
from 8.00 to 19.00, by phone:
+38 (096) 757-90-99.
Candidate of Medical Sciences, Assistant of the Department of Otorhinolaryngology, ONMedU,
doctor — otorhinolaryngologist of the highest category, allergist
-
- Allergist (Immunologist) deals with the diagnosis and treatment of pathologies of the immune system, in particular bronchial asthma, urticaria and other allergic diseases.
- An otorhinolaryngologist (ENT) specializes in diseases of the ear, nose and throat. Diagnoses and treats diseases such as otitis, sinusitis, sinusitis, pharyngitis, laryngitis, rhinitis, tonsillitis.
- Allergist (Immunologist) deals with the diagnosis and treatment of pathologies of the immune system, in particular bronchial asthma, urticaria and other allergic diseases.
Graduated with honors from Odessa State Medical University and master’s degree in otorhinolaryngology (2001 degree).
15-year certificate of endoscopic diagnosis and surgery in older children.
Advanced qualification courses:
- Laser surgery of ENT organs, head and neck” in 2000 (m.Berlin, Nіmechchina).
- «Endoscopic surgery of the nose and paranasal sinuses» under prof. S.Z. Piskunov in 2001 (m. Kursk, Russia).
- «Microsurgery of the ear» — under the supervision of prof. Yu.A.Sushko and O.N. Borisenko, NDI of otorhinolaryngology (city of Kiev).
Scientific activity:
- Double winner of the Olympiad for Young Otorhinolaryngologists under the International Academy of Otorhinolaryngology ї, Head and Neck Surgery (IAO-HNS).
- Laureate of the award «Odesit to rock 2000» in the nomination «young people of ideas to rock».
- Author of 30 scientific works and 3 rational propositions.
Internship for specialty:
- ENT department of Balcali University Clinic, Cukurova University, p. prof. Levent Soylu (m. Adana, Turkey) at 1999 r.
- ENT Department of Charite University Clinic, Oleksandr Humboldt University, prof. Volker Jahnke (m. Berlin, Nіmechchina) in 2000
- ENT Department of the Steiglitz University Clinic, Vilniy University, prof. Hans Sherer (m. Berlin, Nіmechchina) in 2000 rotation.
- Mayo Clinic Arizona (USA) 2012 Transoral surgery of the head and neck.
- Austria. Graz-course of nasal endoscopy. 2013
- Received the Kingdom of Great Britain and Irish Ireland. Cambridge. University spital. Endoscopic surgery — dissection course 2014
- Pediatric anesthesiologist — resuscitator at the ENT Clinic of Dr.

 As discussed, any green vaginal discharge is a ‘NO’
As discussed, any green vaginal discharge is a ‘NO’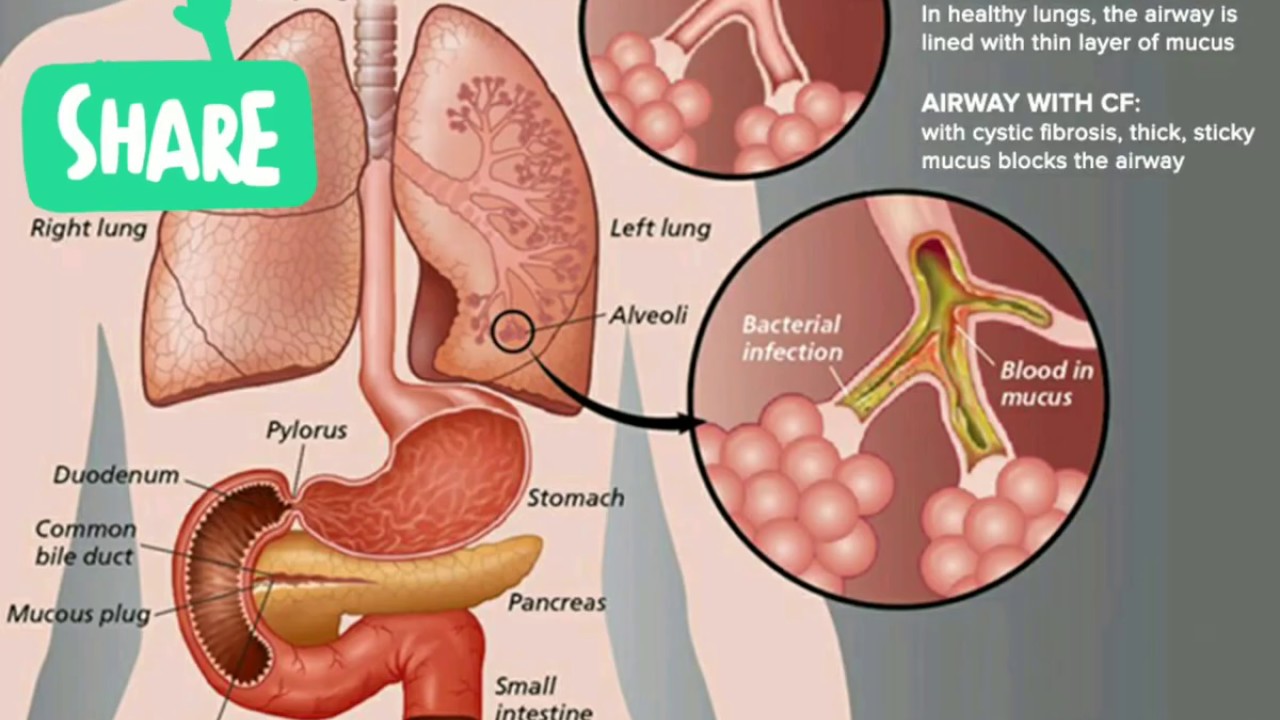
 M. Treatment of diseases of the ENT organs. The latest reference book // Phoenix, 2007.
M. Treatment of diseases of the ENT organs. The latest reference book // Phoenix, 2007.